Von Willebrand disease (VWD) is the most common hereditary coagulation abnormality, presenting in an estimated 1% of the population [1, 2, 3, 4, 5, 6]. In those with VWD, there is a deficiency or dysfunction of von Willebrand factor (VWF), a plasma protein that controls platelet haemostatic function and stabilises blood clotting with factor VIII (FVIII). Those with VWD often experience symptoms related to mucosal bleeding, with VWF levels greatly affecting the amount of bleeding experienced. Symptoms include epistaxis, gingival bleeding, menorrhagia and easy bruising. Women tend to have more intense symptoms than men, mostly relating to their menstrual cycle [1, 2, 3, 4, 5, 6, 7].
Gingival bleeding is often reported in those with VWD, but recent efforts have been made to determine whether gingival bleeding is a true symptom and result of VWD. Studies examining the relationship between VWD and gingival bleeding have conflicting results; however, this may be due to indirect effects of VWD on confounding factors such as oral hygiene. For example, a study by Urdaneta and colleagues found that those with VWD had significantly more plaque and poorer oral hygiene than those without VWD [3].
Research has shown that many patients with bleeding disorders have a fear of performing tasks that may increase bleeding, such as removing plaque with brushing and flossing. Consequently, it has been reported that patients with bleeding disorders generally have poorer oral hygiene than those without bleeding disorders [3]. Research has also shown a relationship between the presence of plaque and a higher risk for dental caries (cavities) and periodontal (gum) disease [8, 9, 10, 11, 12]. Therefore, if those with VWD are not properly removing plaque due to fear of causing gingival bleeding, they are putting themselves at a higher risk of developing dental caries and periodontal disease.
Dental caries in permanent teeth is the most prevalent disease worldwide. The presence of dental plaque on the tooth is necessary for a cavity to form [9]. When carious lesions (cavities) are not addressed, there is potential for the lesion to extend deep into the nerve of the tooth, causing a systemic infection and/or causing the need for an extensive restoration or removal of the tooth itself.
Under the umbrella of periodontal diseases, gingivitis and periodontitis are the most prevalent diseases of the periodontium, the soft and hard tissues that surround the tooth. Alarming data from the National Health and Nutrition Examination Survey (NHANES) shows that 47.2% of American adults have periodontitis and even more American adults have gingivitis [8]. Gingivitis and periodontitis are caused primarily by the presence of bacterial plaque and bleeding is often the first sign of periodontal disease. [9, 10, 11, 12, 13]
Gingivitis is typically characterised as bleeding, redness and swelling of the gingiva. When gingivitis progresses into the other supporting structures of the periodontium, periodontitis occurs, causing destruction of the bone that surrounds the teeth and leading to mobility and eventual tooth loss. Though this process typically takes years to cause tooth loss, it is typically related to the amount of plaque present on the tooth surface [9, 10, 11, 12, 13]. Other factors, such as age, social habits, medical conditions, medications and genetic factors also play a role [8]. Scientific evidence shows a correlation between periodontal disease and systemic conditions such as heart disease, stroke and diabetes [9, 10, 11, 12, 13].
In addition, those with VWD (along with other bleeding disorders) are at higher risk for severe treatment complications, especially after dental treatments such as extractions and local anaesthesia [14, 15, 16]. Patients with VWD therefore require dental treatment accommodations. However, this bleeding disorder is unfamiliar to many oral health care providers and many do not have experience in treating patients with coagulation disorders, especially VWD [3,14,16,17].
Due to the increased risk of treatment complications in VWD patients, preventive dentistry and oral health education is of great importance in order to minimise the need for extensive dental procedures. Efforts are being made to address this issue in the US. For example, in the United States some bleeding disorder clinics have a dental hygienist available during the clinic appointment to review oral health education with those with VWD and their oral healthcare providers, enabling the safe and effective treatment of these patients [3,14,16,17]. In the state of Michigan the majority have a DH as an active member of the hematology team. One of the early signs of periodontal disease is bleeding gums; thus, monitoring for gingival bleeding can be helpful in detecting and treating oral disease in its early stages. However, patients with VWD may have excessive gingival bleeding due to the lack of VWF. In order to implement preventive oral health measures in this patient population effectively, it is therefore important to first understand the effect of VWD on gingival bleeding.
The purpose of this cross-sectional pilot study was to determine the relationship between VWF levels and gingival bleeding when controlling for possible confounding variables, including age, plaque, oral hygiene habits and dental care utilisation. By understanding the relationship between VWD and gingival bleeding, providers will be able to better address oral hygiene as a preventive agent for periodontal disease. In addition, the study sought to determine the effectiveness of having a dental hygienist at bleeding disorder clinics to provide oral health education.
Materials and methods
Women aged 18 or older with VWD were eligible to participate in the study if they had at least 12 teeth present and were capable of providing informed consent. The study focused on women because of the detrimental effects that VWD has on women related to menstrual bleeding [7]. Exclusion criteria comprised those with uncontrolled diabetes, significant psychiatric illness that would interfere with the completion of the survey, or taking medications that cause gingival enlargement (eg calcium channel blockers, anti-seizure medications and immunosuppressants).
Variables and instruments used
Informed consent was documented prior to any data collection. After reading and signing the informed consent document, a 34-question survey was given to the participant to fill out. The survey asked questions about demographics, social behaviours, how often oral hygiene is reviewed at the individual’s bleeding disorder clinic appointment, perception of oral health, oral hygiene habits, dental care utilisation, and potential issues around access to dental care.
A clinical oral examination was performed to assess the amount of plaque and gingival bleeding. Data was gathered on the six Ramfjord teeth – designated teeth that are likely to give a good representation of the entire mouth for data collection purposes (teeth numbers 3, 9, 12, 19, 25, and 28) [18]. Presence of plaque was documented as 1, and no plaque was documented as 0. The gingival bleeding index was used to detect gingival bleeding on the six Ramfjord teeth [18]. This was assessed by employing a gentle C-wrap floss technique subgingivally, then assessing the presence or absence of bleeding. Absence of gingival bleeding was recorded as 0, and the presence of gingival bleeding was recorded as 1. Data was collected on 12 surfaces, with a total of two surfaces per tooth.
Information from the patient’s medical chart recording the patient’s most recent VWF levels and date, treatment for VWD, other medical conditions and other medications was also gathered.
Sample size estimation
The study was designed to achieve at least a 45% difference in the occurrence of gingival bleeding when plaque is present in the twelve sites measured for the study. A power calculation was generated. Based on a study by Pizzo et al., it was determined that a sample size of 38 women would provide for at least 80% power that there would be a 45% or greater incidence of gingival bleeding when plaque is present [19].
Statistical Analysis
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) program, version 19.0 for Windows. Paired samples t-tests, logistic regression and multiple linear regression models were used to analyse the data gathered. All results were considered significant for a level of α<0.05.
Results
Descriptive statistics
A total of 44 women with VWD who met all the eligibility criteria completed the study. The majority were between the ages of 18 and 30, Caucasian, unemployed and had dental insurance. The average age was 39.1 +/- 15.8. The majority were non-smokers and used alcohol. Most participants had an education level of high school and/or some college. The descriptive characteristics of the 44 women subjects in the study are shown in Table 1.
Table 1
Demographics of sample
The majority of participants attend the bleeding disorder clinic at Michigan State University. 65% stated that oral hygiene is reviewed at their bleeding disorder clinic appointments frequently or at every visit. Only 15% of individuals stated that oral hygiene was never reviewed at these appointments. This was not specific to the clinic in which the individual attended. Of those surveyed, 57.5% stated that a dental hygienist at their bleeding disorder clinic is the primary provider that reviews oral hygiene education (data not shown).
Data regarding perception of oral health, self-reported gingival bleeding and oral hygiene habits is shown in Table 2. Although 73.8% of the women surveyed have dental insurance, only 56.1% had attended a dental appointment within the last six months. For 29.3% of women, it had been more than a year since their last appointment with a dentist. Open-ended questions were used to assess whether potential issues around access to dental care existed. The responses to these questions can be found in Table 3.
Table 2
Perception of oral health, importance of oral health, frequency of gingival bleeding and oral hygiene habits
Table 3
Possible complications interfering with access to dental care for women with von Willebrand disease (VWD)
For data analysis purposes, the patients’ VWD severity was classified into three groups, according to their most recent VWF reading, as follows: 1= VWF less than or equal to 30; 2= VWF 31-60; 3= VWF higher than 60. Of the women who participated in the study, 16.3% had a VWF level of less than or equal to 30, 14% had a VWF level between 31 and 60, and 53.5% had a VWF level of more than 60. Although a VWF level of greater than 60 is considered to be at the lower end of normal, as previously stated, VWF levels can fluctuate in times of stress, exercise and hormonal changes. Data were missing on five individuals as lab values for VWF were not present in their medical charts.
Clinical measures
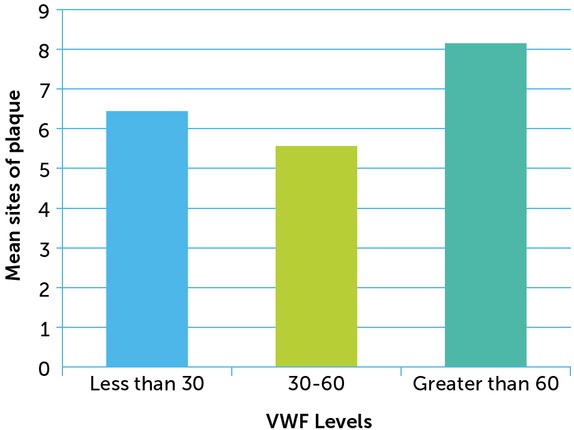
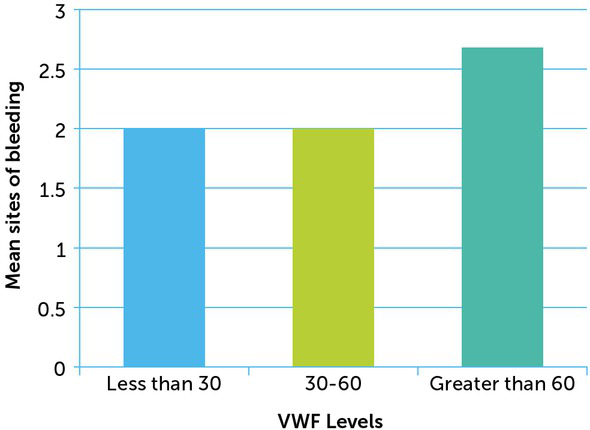
On average, women had 7.34 (SD=4.46) sites of plaque and 2.41 (SD=2.55) sites of bleeding out of a possible 12 sites. The clinical data is shown in Table 4. When the data was stratified by VWF levels, it was also found that those with lower levels of VWF have less plaque and less gingival bleeding than those with closer to normal VWF levels. A visual representation of this data is shown in Figures 1 and 2.
Table 4
Frequency table: number of sites with plaque and bleeding of 12 sites measured per person
| NUMBER OF SITES WITH PLAQUE | FREQUENCY | PERCENTAGE (%) |
|---|---|---|
| 0-4 | 12 | 27.4 |
| 5-8 | 7 | 15.9 |
| 9-12 | 25 | 56.8 |
| NUMBER OF SITES WITH BLEEDING | FREQUENCY | PERCENTAGE (%) |
|---|---|---|
| 0-4 | 34 | 77.3 |
| 5-8 | 9 | 20.5 |
| 9-12 | 1 | 2.3 |
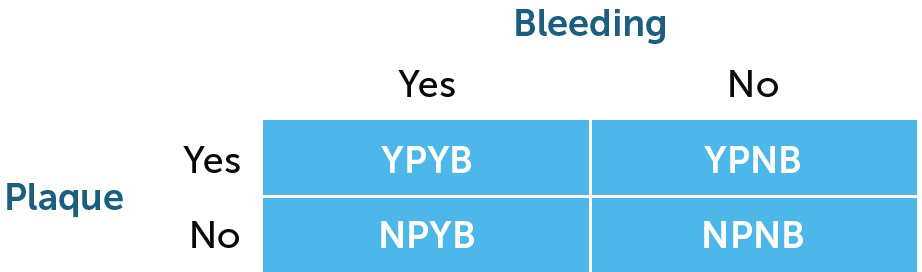
To determine the relationship between plaque and gingival bleeding, each site in the mouth had one of four possible outcomes, as follows:
On average, 44.33% (n=5.32) of the 12 sites had plaque, but no bleeding; 35.58% (n=4.27) of the 12 sites had no plaque and no bleeding; 16.25% (n=1.95) of the 12 sites had plaque with bleeding; and only 3.75% (n=0.45) of the 12 sites had no plaque with bleeding (see Table 5).
Table 5
Average number of sites (of 12 sites measured) and standard deviations for each possible clinical outcome (Y=Yes, N=No, P=Plaque, B=Bleeding)
| MEAN | SD | |
|---|---|---|
| YPYB | 1.95 | 2.27 |
| YPNB | 5.32 | 4.36 |
| NPYB | 0.45 | 0.76 |
| NPNB | 4.27 | 4.31 |
When examining the effects of plaque on gingival bleeding, two main questions were tested with data analysis. Firstly, the number of sites that had plaque with bleeding (YPYB) was compared to the number of sites that had bleeding but no presence of plaque (NPYB). This answered the question “When bleeding was noted, is the bleeding more related to the presence of plaque or not?” Secondly, the number of sites that had plaque with bleeding (YPYB) was compared to the number of sites that had plaque with no bleeding (YPNB). Comparing these two measures provided the answer to the question “When plaque was present, is the site likely to have gingival bleeding or not?”
Statistically significant differences were noted between the mean differences in YPYB vs. NPYB and YPYB vs. YPNB groups when assessed using paired sample t-tests (p<0.001), (see Table 6). This shows that when there is plaque present on a surface, it is more likely not to bleed when using the gentle C-wrap flossing technique. Though studies have shown the relationship between plaque and gingival bleeding, low amounts of gingival bleeding were noted when using the C-wrap technique in this group, even with the presence of plaque. The second test shows that when gingival bleeding is noted, it is more likely due to the presence of plaque. Linear regression was used to determine whether VWF level had a significant effect on the relationship noted. In both tests, VWF was not a statistically significant confounding variable (p>0.05), as shown in Table 6.
Table 6
Difference in means between possible outcome pairs, with significance for paired samples t-test and when using linear regression to control for VWF level
As an inverse relationship was noted, in that those with closer to normal VWF levels presented with more gingival bleeding, multiple linear regression was used to test for possible confounding variables. In the model shown in Table 7, age is shown to have a protective effect on the number of sites with gingival bleeding. Time since last dental visit also had a significant effect on the relationship, showing that when an individual does not visit the dentist every six months, the average number of sites with gingival bleeding increases significantly (p=0.044).
Table 7
Multiple linear regression model for bleeding in women with VWD. Dependent variable: gingival bleeding
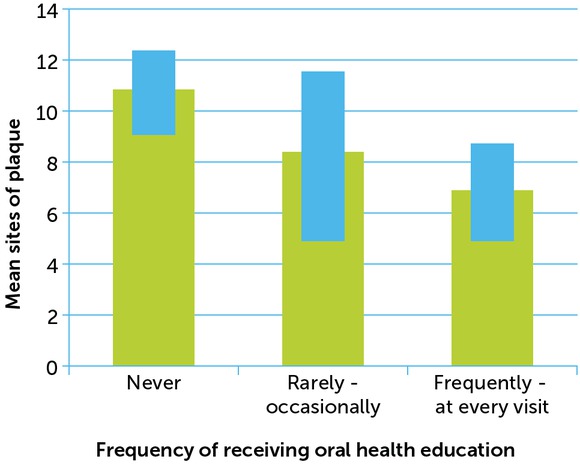
Since plaque had a larger effect on gingival bleeding than VWF, the effectiveness of providing oral health education was analysed. Linear regression was used to determine whether the frequency of oral health education played a role in the amount of plaque noted. For those who stated that they never received oral health education at their bleeding disorder clinic, plaque was present on 10.5 of the 12 sites measured. In those women who stated that oral hygiene education was reviewed at every visit, plaque was present on 6.8 of the 12 surfaces measured. This difference in the amount of plaque was statistically significant (p=0.03), as seen in Figure 3.
Discussion and conclusion
To the authors’ knowledge, this was the first study to assess the relationship between VWF levels, plaque accumulation and gingival bleeding when controlling for other possible confounding variables. Previous studies have compared plaque presence and gingival bleeding in healthy individuals to those with VWD, but none have controlled for varying VWF levels or used plaque as a confounding variable for gingival bleeding [3,14,15,22]. This study sought to assess whether gingival bleeding was related to plaque even while controlling for possible confounding variables such as VWF levels, oral hygiene habits, demographics, access to dental care, and self-reported gingival bleeding.
For this particular study, severity of VWD was controlled for in the analysis to determine whether there was a trend between more bleeding sites and decreased VWF. The relationship between VWF level and gingival bleeding sites was first tested with linear regression. This relationship was not significant, prompting the need to test confounding variables. Age and last dental appointment seemed to have a greater effect on the amount of gingival bleeding noted in each patient. Though not a statistically significant relationship, the amount of gingival bleeding decreased as age increased. Having a dental visit within the past six months had a protective effect on the amount of bleeding.
Comparison and analysis of the means of these four outcomes indicated that the presence of plaque may be more significant in causing gingival bleeding than low VWF. In fact, the majority of sites in the population involved in the study had plaque presence, but no concomitant bleeding. This study shows that there is 95% confidence that among women with VWD, the average number of sites with gingival bleeding is between 1.60 and 3.19 of 12 sites measured. The fact that a greater number of sites had no bleeding, even with presence of plaque, indicates that women with VWD can perform gentle C-wrap flossing without causing gingival bleeding, suggesting that performing normal oral hygiene interventions would not adversely affect their bleeding control. Expressing this confidently to patients with VWD can assure them that it is possible to perform proper oral hygiene effectively without causing excessive, if any, gingival bleeding.
When examining the amount of gingival bleeding and determining confounding variables related to delivering oral hygiene instruction, two questions on the patient survey were examined. The first asked, “How often does someone at your bleeding disorder clinic discuss oral health with you?”; the second asked, “Who usually discusses the importance of oral health with you?” Both variables were used to analyse the effectiveness of having a dental hygienist at bleeding disorder clinics. Results showed that there is a significant difference in both presence of plaque and gingival bleeding when controlling for these two variables. This may imply that educating patients on oral health can result in improved oral hygiene, leading to a decreased risk of developing periodontal disease. As previously stated, other confounding factors influence the development of periodontal disease as well, including, but not limited to medication, genetics, and age.
There were several limitations to the study, mostly related to limited time and resources. A longitudinal study would have been beneficial to evaluate the effects of the fluctuation of VWF levels over time [16,20]. A larger sample size would have given the study more power.
One major limitation was the lack of a true control group. In the hope of addressing this, data from the study was compared with data from the National Health and Nutrition Examination Survey (NHANES) to determine whether the presence of gingivitis differed in women with and without VWD [21]. A chi-square test was used to compare the presence of gingivitis in women with VWD and the presence of gingivitis in women from the NHANES data. When cases were weighted by N, the difference in the percentages was not significant (Pearson’s Correlation: 0.169), as shown in Table 8.
Table 8
Chi-square test for gingivitis in women from NHANES and women with VWD
| NUMBER (PERCENT (%)) GINGIVITIS | ||
|---|---|---|
| Study | Yes | No |
| NHANES | 1996 | 2173 |
| (47.9) | (52.1) | |
| VWD | 20 | 16 |
| (55.6) | (44.6) | |
Another limitation was the index used to measure presence of plaque. As the results showed that plaque was present on the majority of sites with no bleeding noted, an index measuring the amount of plaque present would have been beneficial in order to give insight into how long the plaque was present, contributing to its thickness.
Conclusion
In summary, this study found that VWF levels do not have a significant effect on the amount of gingival bleeding present, but that gingival bleeding is more a result of poor oral hygiene and lack of dental care. Sharing this information with individuals that have VWD can help them understand that gingival bleeding is not due to the bleeding disorder itself, but from not properly removing plaque. It is imperative that the VWD population understand the aetiology of periodontal disease and that, rather than being the result of low VWF levels, gingival bleeding is a sign of periodontal disease.
The study also found that the inclusion of a dental hygienist in the comprehensive team at bleeding disorder clinic may lead to improved patient oral hygiene. Ultimately, as gingival bleeding in women with VWD has been shown to be minimal and related to the presence of plaque rather than being a direct result of low VWF levels, practicing routine oral hygiene is safe and recommended in this patient population. As many women with VWD have felt bias or have been refused treatment by oral healthcare providers, the dental hygienist serves as an important liaison between the patient, the dentist and the bleeding disorder clinic. In addition, the hygienist communicates with the haematologist, explaining dental procedures so that appropriate medical recommendations can be made, thereby reducing the incidence of dental treatment complications. Improving oral care and decreasing gingival inflammation can ultimately reduce the risk of oral systemic disease.