Haemophilia and associated bleeding disorders are chronic conditions that require easy, accessible, and reliable venous access for treatment. Peripheral venous access is traditionally the first option considered for prophylaxis.
Prophylaxis was introduced in Sweden in 1958 in order to prevent joint bleeding, which in turn progresses to the development of arthropathy. It is initially introduced to children with bleeding disorders during the first two years of life and peripheral venous access at this age can be problematic [1,2ome environment. Central venous catheters (CVC), in particular port-a-caths, are widely used to facilitate home treatment in young children; however, these devices require surgical insertion and are not without their own complications, including repeated infections, thrombosis and body issues in girls facing puberty [3,4,5]. Nevertheless, peripheral access and CVC remains the route of choice in paediatric venous access [3].
An arteriovenous fistula (AVF) is an abnormal connection between an artery and a vein and offers another form of venous access. AVF has been used in a number of haemophilia centres in Europe, and have been found to be an ‘attractive solution’ [4]. Studies on use of AVF in patients with bleeding disorders have shown them to be less problematic compared with CVCs [4, 5, 6]. In this report we describe our experience with the use of AVF for routine venous access in three children with severe inherited bleeding disorders.
Materials and methods
Data were collected on venous access methods used at the paediatric centre at the Evelina London Children’s Hospital. 242 children are registered at the comprehensive care centre, 48 of whom have a severe bleeding disorder. Of these, 27 have a CVC currently (PICC n=1, port-a-cath n=25, Hickman line n=1) and 3 have an arteriovenous fistula (AVF). Patients with AVF include two boys and one girl:
Patient 1 is a 12 year-old Caucasian boy with severe haemophilia A, who sustained a traumatic intracerebral bleed, subsequently leading to quadriplegic motor disorder from the age of 9 months. He remains on prophylaxis with recombinant factor VIII (rFVIII). As a result of repeated port-a-cath infections and poor venous access, an AVF was fashioned 5 years ago. The procedure was uneventful and covered with rFVIII concentrate.
Patient 2 is a 7 year-old boy of West African origin with severe haemophilia B and an inhibitor. He requires daily treatment with recombinant factor VIIa (rVIIa). He has also had repeated port-a-cath infections and developed a phobia of needles. He has poor venous access and an AVF was constructed 2 years ago. The initial fistula formation was associated with stenosis in the left fistula vein above the brachiocephalic anastomosis, hence a fistuloplasty was performed by the interventional radiologist. Post-procedure angiography showed satisfactory appearance of the fistula.
Patient 3 is a 12 year-old Asian girl with type III von Willebrand disease and an inhibitor. Due to need for regular factor treatment in the context of poor venous access and the onset of puberty, an AVF was formed under von Willebrand factor cover. The procedure was tolerated well and there were no immediate complications.
Patient characteristics are presented in Table 1. In each case, the AVF formation procedure was performed under general anaesthesia by the paediatric renal transplant surgeon. All three patients had upper limb imaging scans prior to the procedure to evaluate both arterial and venous systems. The procedures lasted an average of 1.5 hours, with a minimum time of 40 minutes and a maximum time of 2 hours, and the patients spent a mean of 3.6 days in hospital (minimum admission time was 3 days, maximum 5 days).
Table 1
Patient demographics
Results
To date, the success rate with all three AVFs at our centre has been 100%. Despite the need for even more frequent venous access at times of bleeding episodes, there have been no problems in the patients accessing the AVF over a follow-up period of 8-69 months. Thus, the AVF in all three patients has proven to be a vital and reliable route of venous access to ensure the administration of prophylaxis, with added ease in locating the AVF as noted in other studies [7].
Discussion
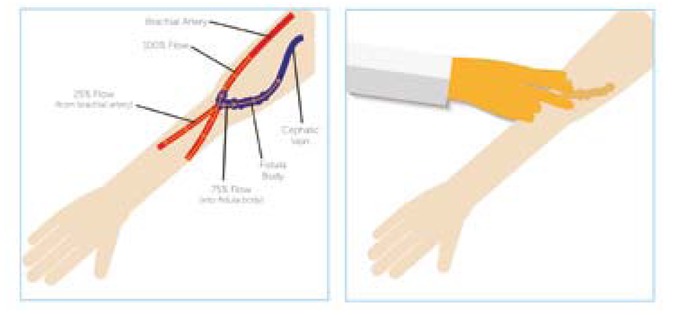
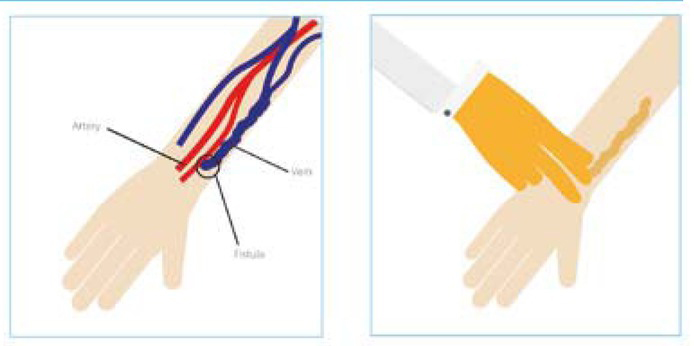
AVF is an anastomosis that redirects arterial blood flow into a vein. In time, it becomes dilated due to the new haemodynamic conditions. Over a period of 6-12 weeks the lumen of the vein widens, thus enabling the venous blood flow to increase [10]. The vein then becomes suitable for puncture and the use of prophylaxis or other alternative treatment can begin. In haemophilia the brachial artery (Figure 1) is preferred for use, as research suggests that the radial artery (Figure 2) is related to a higher rate of failure [6]. AVF is the recommended vascular access for haemodialysis patients; however, it is now becoming an increasingly viable alternative form of access, for the use of prophylaxis in haemophilia and other related bleeding disorders [8,9,14].
AVF access
We acknowledge that our report is based on very few patients. However, all three patients have achieved a success rate of 100% at a follow-up period of 8-69 months and no further complications have been found. We have found AVF to be a valuable substitute in achieving effortless venous access, in particular for children who have suffered repeated port-a-cath infections and those with poor superficial venous access [1]. Modern prophylaxis management in haemophilia and associated bleeding disorders relies on easy venous access to administer treatment and it is essential to be able to comply with treatment regimens. Traditionally in haemophilia and related bleeding disorders, peripheral access and central venous catheters (CVC), such as port-a-caths, are used in the administration of prophylaxis [11], methods of venous access which have their own complications.
In a three-year study of 27 patients, Santagostino et al. found that AVFs were accepted readily, as treatment became attainable with ease of access [7]. Parents in particular have benefited from this, finding independence in treating their children at home and reducing hospital attendance for venous access [6,14].
Other studies of the use of AVF may also prompt comprehensive care centres to re-evaluate the use of alternate methods as a form of regular access for the treatment of bleeding disorders. Al-Jaishi et al, suggest that AVFs are confirmed to have an exceptional history in long-term patency and durability, with minimal complications [4, 16,15]. Mancuso et al. propose that AVFs are viable and painless alternative, preferred both by patients and health care professionals due to lower rates of infection compared to CVCs [6]. A further advantage cited by the authors is that AVFs are easy to use in the home environment and easily accepted by patients. Increased volume/dose may also be infused through an AVF and is particularly advantageous in ITI patients [5, 8].
Although the AVF is a viable alternative option for intravenous access in haemophilia, it is not without problems. AVFs have to be constructed under general anaesthesia, exposing the patient to the potential complications associated with anaesthesia. The flow of the AVF must be assessed monthly until maturation, which can take 6 to 12 weeks, impacting school attendance [18]. Complications such as local haematomas at the AVF site, distal steal syndrome, loss of AVF patency, blood overflow, aneurysmal dilatation and inadequate or unsuccessful maturation may occur, which may prevent successful AVF use [5,6,8]. It is also important to note that blood pressures and blood draws should be avoided, on the arm of the AVF and tourniquets may only be applied gently for a brief period to facilitate effortless AVF access [9,17].
While AVF is not the most straightforward option, it could benefit certain patients. Further evidence on the long-term use of AVF in paediatrics will help clinicians, patients and carers in making informed decisions.
Conclusion
Research has shown that AVFs are durable and have the capacity to facilitate repeated venous access with a decreased incidence of infection, compared to that of indwelling central venous access devices [4,18]. Our experience suggests that AVF is a viable option for venous access in patients with haemophilia and other bleeding disorders, and particularly for children with repeated CVC infections or poor peripheral venous access.