In the UK, the introduction of replacement factor concentrates has had an enormous impact on the well-being and life expectancy of those with bleeding disorders. Prior to the introduction of adequate treatments, many people with haemophilia died before reaching adulthood [1]. With advances in treatment and care, children born with haemophilia in the United Kingdom (UK) today have a normal life expectancy [2]. As we now also have an ever-increasing older population, it is now appropriate to consider the numerous health issues associated with this in relation to haemophilia. As studies have reported that people with haemophilia have an increased risk of hypertension, this is a particular area of interest [3, 4, 5].
Hypertension is a well-known risk factor for ischaemic heart disease and cerebrovascular events. Strokes are known to be the second leading cause of death in the over-60 age group [6]. Globally, strokes affect 15 million people per year; of these, 6 million people die and 5 million are left permanently neurologically impaired [6].
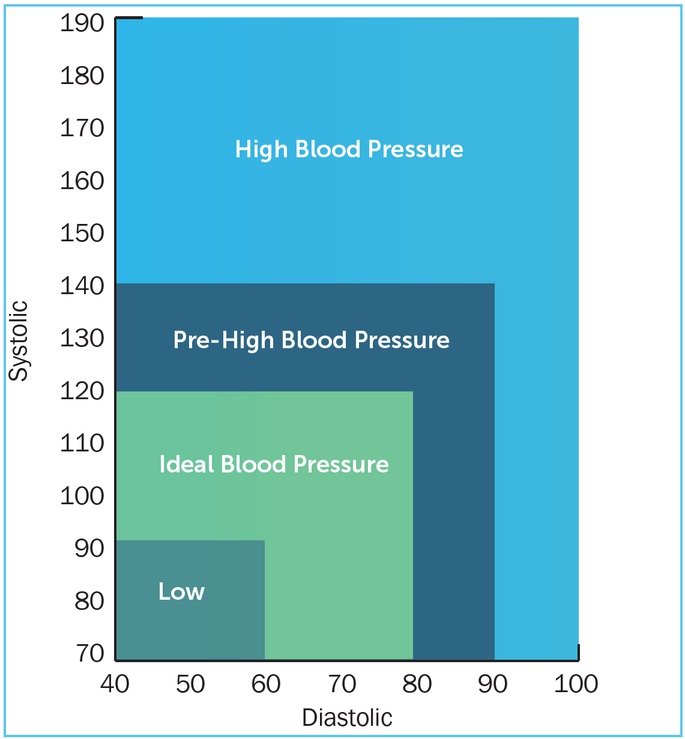
Blood pressure measurements should now be done routinely on all adult patients as part of their care when attending haemophilia clinics [4]. High blood pressure in adults is defined as a reading over 140/90 mmHg (see Figure 1) [7]. Obesity, lack of exercise, smoking and alcohol intake can all contribute to a raised blood pressure. However, it is the intake of sodium in salt that is credited with being the major contributing factor in hypertension [8].
Figure 1:
Classification of blood pressure for adults (from www.bloodpressureuk.org/BloodPressureandyou/Thebasics/Bloodpressurechart)
Salt is made up of 40% sodium and 60% chloride by weight. Sodium (Na) is an electrolyte which helps to maintain blood pressure, regulate a normal fluid balance, and helps in the transmission of nerve impulses and muscle contractions. Sodium levels are regulated by the kidneys and adrenal glands, which control whether the body stores the sodium or excretes it into the urine [8]. Sodium is found naturally in most foods, and is often added to food products in the form of monosodium glutamate (MSG), sodium nitrate, sodium saccharin, sodium bicarbonate and sodium benzoate [9].
There is much debate about the recommended daily amount of salt that an adult should consume, the World Health Organisation (WHO) recommends < 2g/day sodium (5g/day salt) [10]. To put this into perspective, 1 teaspoon of table salt contains 2.3g of sodium. For healthy adults up to 50 years of age, the recommended salt intake is between 1.5g-2.3g sodium per day. For adults over 50 years of age, it drops to 1.3g per day; and for the over-70s it is about 1.2g a day [11]. Adults with high blood pressure should have no more than 1.5g per day [12]. The UK Government has embarked upon extensive campaigns to alert the general public of the need to reduce their daily salt intake. In the UK, the average salt intake is approximately 8.6g of salt daily. A reduction in salt intake is associated with lowering blood pressure within 4 weeks [13].
Thus, sodium, although essential for our health and well-being, can also have a detrimental effect on health if consumed excessively. A reduction in daily salt intake is recommended for the older population, and especially for people of South Asian or Black African ethnicity as these groups are recognised as having an increased sensitivity to salt [8]. It is estimated that by reducing global salt consumption to the recommended level, 2.5 million deaths could be prevented each year [8]. Reducing salt intake should therefore be taken seriously by everyone. The National Institute of Clinical Excellence (NICE) is currently aiming to reduce the maximum intake of salt in adults in the UK to 6g per day by 2015, with further reductions to 3g by 2025 [14]. The recommended salt intake for children varies according to age (Table 1).
Table 1:
Recommended salt intake for children
| Age | Maximum salt intake |
|---|---|
| 0-6 months | <1g / day |
| 6-12 months | 1g / day |
| 1-3 years | 2g / day |
| 4-6 years | 3g / day |
| 7-10 years | 5g / day |
| 11 years and above | 6g / day |
Following the introduction of replacement clotting factors, the lives and life expectancy of people with bleeding disorders have improved considerably. It is therefore now appropriate to consider whether factor concentrates have undesirable effects which were not previously relevant.
As can be seen in Table 2, the levels of sodium in different factor concentrates can vary considerably. For those patients who have a history of hypertension, it may be pertinent to consider this information when prescribing factor products. There are industry guidelines regarding the packaging and labeling of medication to ensure clarity and to enable medicines to be used safely [15]. The British Heart Foundation states that: “All medicines that contain at least 1mmol (or 23mg) of sodium - a component of salt - in each dose are required to declare on their labelling that the product contains sodium” [16]. However, there seems to be no consensus on how this information should be represented, potentially leading to difficulties in how it is interpreted. For instance, different factor products display sodium levels in mmols, mgs, mEq or as a percentage. This lack of consistency could increase confusion regarding sodium content and makes the direct comparison of factor products difficult in this respect. The data in Table 3 makes it clear that factor replacement products do contain sodium, some in significant levels. As such, haemophilia practitioners should have increased awareness of this issue.
Table 2
Factor concentrates and their sodium levels based on information obtained from the Medical Information Departments of individual pharmaceutical companies producing factor products.
| Name of factor | Sodium level |
|---|---|
| Advate | 10mg per vial* |
| Alphanate | 230mg per 1,000 IU vial |
| Benefix | <23mg per vial* |
| DDAVP (4mcg/ml) | 9mg per ml |
| DDAVP nasal spray | 7.5mg per ml |
| Fandhi | <23mg per 1,000 IU vial |
| Feiba | 80mg per 500 IU and 1,000 IU vial 200mg per 2500 IU vial |
| Haemate P | 70mg per 1,000 IU vial |
| Helixate Nexgen | 23mg per 1,000 IU vial |
| Kogenate | 23mg per 1,000 IU vial |
| Novo 7 | 5.84mg of sodium per 1.2mg Novo 7 |
| Refacto AF | 29mg per vial* |
| Voncento | 29.5mg per 1,000iu/2400 IU vial |
| Wilate | 117.3mg per 1,000 IU vial |
Table 3:
Factor concentrates and their sodium levels per 3,000 IU of factor concentrate, based on information obtained from the Medical Information Departments of pharmaceutical companies producing factor products
| Name of factor | Sodium level | Sodium level on administration of 3,000 IU factor concentrate according to vial used | |
|---|---|---|---|
| Example | Total sodium | ||
| Advate | 10mg per vial* | 3 x 1000 IU 6 x 500 IU | 30mg 60mg |
| Alphanate | 230mg per 1,000 IU vial | 3 x 1000 IU | 690mg |
| Benefix | <23mg per vial* | 3 x 1000 IU | <69mg |
| Fandhi | <23mg per 1000 IU vial | 3 x 1000 IU | <69mg |
| Feiba | 80mg per 500 IU and 1000 IU vial 200mg per 2500 IU vial |
2500 IU+ 500 IU 3 x 1000 IU 6 x 500 IU |
280mg 240mg 480mg |
| Haemate P | 70mg per 1000 IU vial | 3 x 1000 IU | 210mg |
| Helixate Nexgen | 23mg per 1000 IU viall | 3 x 1000 IU | 69mg |
| Kogenate | 23mg per 1000 IU vial | 3 x 1000 IU | 69mg |
| Refacto AF | 29mg per vial* |
3 x 1000 IU 6 x 500 IU |
87mg 174mg |
| Voncento | 29.5mg per 1000 IU/2400 IU vial | 3 x 1000 IU | 88.5mg |
| Wilate | 117.3mg per 1000 IU vial | 3 x 1000 IU | 35.19mg |
Some vials of factor concentrates have the same quantity of sodium, irrespective of the amount of factor concentrate they contain, e.g. 500 IU or 1,000 IU. The total amount of sodium administered can therefore vary significantly, depending on the size of the vials used to make up the required amount of factor concentrate (see Table 3). As noted above, it is recommended that the maximum daily intake of sodium for healthy adults is between 1.5g-2.3g, and less than 1.5g for those with hypertension. Whilst some products contain as little as 30mg of sodium per 3,000 IU of factor concentrate, others contain 690mg of sodium per 3,000 IU of factor concentrate. Therefore, depending on the choice of factor concentrate prescribed, the vial sizes used and the frequency of administrating the dosage to achieve haemostasis, this could significantly contribute to the overall daily sodium intake. This may be particularly significant for children undergoing immune tolerance induction therapy due to the frequency of administration of factor concentrates. There could also be a cumulative effect, contributing to the increased incidence of hypertension in adults.
Other factors, such as obesity, lack of exercise, smoking and alcohol intake, can contribute to hypertension. Foods high in potassium may help to reduce the adverse effects of sodium on blood pressure [17]. Health professionals should be proactive in promoting a healthy diet, rich in fruit and vegetables and low in saturated fats, and in encouraging people to be physically active and stop smoking, as these will also help to reduce blood pressure [18]. Being aware of the sodium levels in replacement products may also help health professionals to make informed choices for individuals who need to reduce their sodium intake.
Blood pressure is routinely monitored when patients attend their haemophilia centre for review. Readings should be communicated to general practitioners (GPs) as they are responsible for management of blood pressure. Regular liaison between haemophilia centres and the patient’s GP will enable provision of the best care for patients. In addition, studies are needed to clarify the prevalence of hypertension in the UK haemophilia population and to establish whether lifetime exposure to replacement clotting factors results in an increased risk associated for hypertension.