Haemophilia is an X-linked recessive bleeding disorder caused by a deficiency of coagulation factor VIII (FVIII) (in haemophilia A) or factor IX (FIX) (in haemophilia B). Bleeding severity correlates with the level of clotting factor; those with the lowest clotting factor levels (<0.01 IU/dL) suffer significant spontaneous bleeding into the large synovial joints (knees, elbows and ankles) of the musculoskeletal system. Over time, joint bleeds result in irreversible joint damage and functional limitations [1,2]. Typically joint bleeding starts in early childhood and initial joint changes may be subclinical, with the consequences not apparent until adulthood [3].
Prophylactic administration of clotting factor has been shown to prevent the development of joint damage [4,5] and is now accepted as the standard of care for children born with severe haemophilia [6]. As a result, boys born with severe haemophilia in the UK are now routinely treated with prophylaxis [7] and are increasingly growing up to be active members of society with near-normal lifestyles and lifespans. Patients with haemophilia receive routine clinical care at either a comprehensive care centre or haemophilia centre, with the recommendation that patients with severe or moderate haemophilia receive reviews on a 6-monthly basis. The clinicians involved include haematologists, specialist nurses, physiotherapists and psychologists. The UK Haemophilia Centres Doctors’ Organisation (UKHCDO) recommends that children receive a standardised joint assessment to monitor joint status [7]. Most haemophilia centres in the UK use a joint assessment score performed by haemophilia physiotherapists, with the majority using the Haemophilia Joint Health Score (HJHS). The HJHS is routinely used at follow-up clinics as long as no bleeds have occurred in the preceding four weeks.
The HJHS Version 2, (HJHSv2.1) is an assessment tool for children. This is a well-validated tool that accurately reflects early joint changes and can be used to monitor joint health, damage and improvement [8, 9, 10]. The HJHS assesses the key joints; ankles, knees and elbows and evaluates flexion, extension, range of movement, muscle strength, swelling, duration of swelling, crepitus, gait, pain and muscle atrophy. It has a total score of 124, where 0 reflects no joint damage and higher scores worsening joint damage. More recently the reliability and validity of the HJHS in teenagers and young men has been explored and found to be excellent [11]. There is a growing use of the HJHS in both child and adult studies [10, 11, 12, 13, 14, 15, 16, 17], even though no studies have reported using the HJHS or any validated joint assessment tool in the older population.
Materials and methods
In May 2013, UK physiotherapists working in haemophilia (n=37) care were surveyed regarding their current practice with respect to joint scoring. The survey was posted on SurveyMonkey and was open to all haemophilia physiotherapists practising in the UK; potential participants were contacted by email and via the Haemnet website (www.haemnet.com). Responses were collected and analysed in June 2013 and discussed at a roundtable meeting. This report is based on the results and discussion.
Results
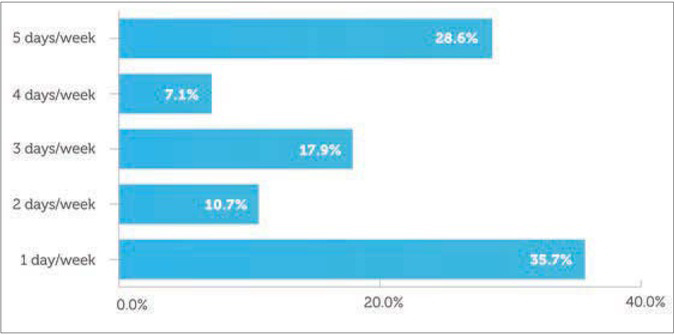
In all, 29 physiotherapists representing three haemophilia centres and 25 comprehensive care centres in the UK responded to the survey. Fourteen centres worked with children only, seven with adults only and eight were combined centres. There was variability in expertise and dedicated time allocated to patients with haemophilia. Only eight respondents worked full time in haemophilia, while 10 worked only one day a week in haemophilia (Figure 1).
Most respondents indicated that they routinely undertook joint scoring, in most cases using the HJHS (83%). A minority (10.3%) were using other scores, such as the Gilbert Score, the Colorado Half Point Score (for adults) and the Haemophilia Chartered Physio Score. Two respondents did not routinely undertake joint scoring.
All respondents stated that, in their hospitals, joint scoring was not performed by non-physiotherapists; indeed, most (95%) felt that joint scoring could not reliably be undertaken by other healthcare professionals.
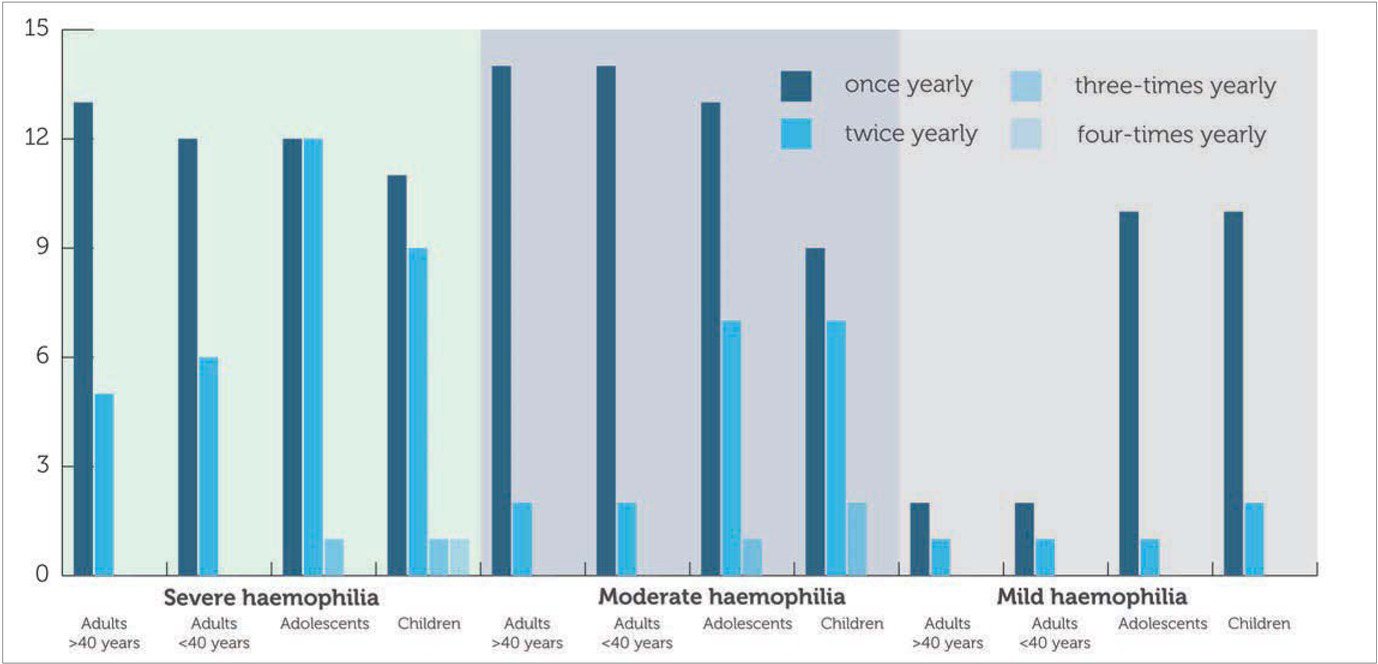
Respondents indicated that most severe and moderate haemophilia patients undergo a joint score assessment at least once a year, although more frequent assessments might be done on children and adolescents (Figure 2). While adolescents and children with mild haemophilia generally received joint scores, adults did not.
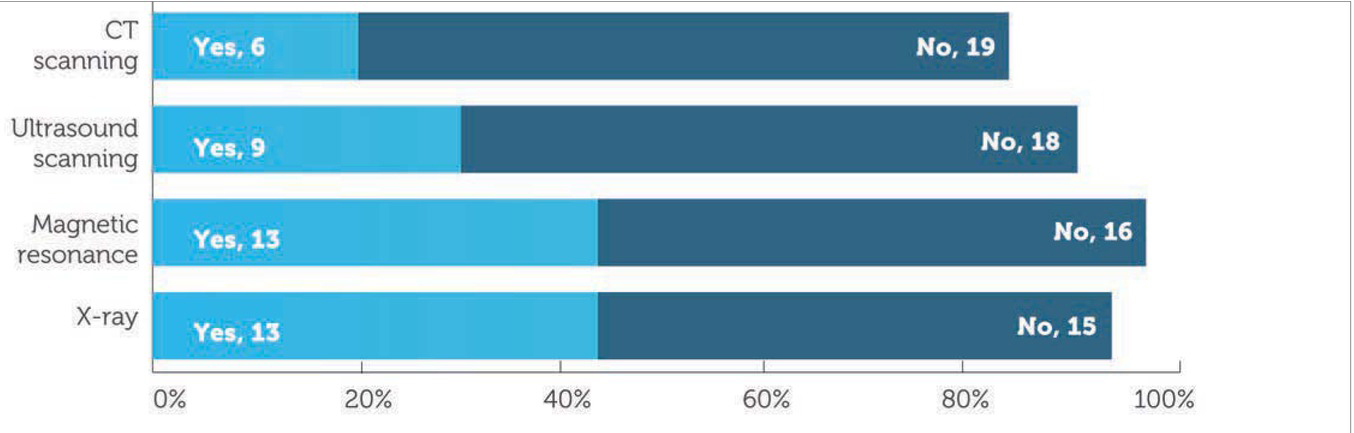
Most physiotherapists were in agreement with the World Federation of Hemophilia (WFH) estimation that joint scoring took less than 90 minutes. Around half of our respondents indicated that their trusts permitted augmentation of joint assessment with other imaging modalities where clinically indicated. X-ray or magnetic resonance imaging assessments were the most widely available, but some physiotherapists had access to ultrasound and CT scanning (Figure 3). Where other imaging modalities were used, these were usually requested by medical staff but it is unclear if this was at the request of physiotherapists.
Although most respondents indicated that joint scores were usually recorded in the patient’s notes, only around half of respondents indicated that the data was also inputted into the UKHCDO’s National Haemophilia Database. One in four physiotherapists (26%) indicated that the joint score data had no direct bearing on the patients’ management plan. However, most (85%) indicated that changes in joint score would be fed back to patients and/or their carers. Most (80%) physiotherapists believed that giving a joint score, whether total or for a particular joint, was beneficial to the individual patient’s concordance with treatment.
While respondents were divided on the question of whether or not the total score reflected total joint health (58% of the sample believed it did not), there was greater agreement that the joint score offered a useful tool for measuring an aspect of overall haemophilia outcomes. Nevertheless, 70% of respondents felt there were better ways of assessing joint health that should be implemented. Free text answers cited gait and movement analysis, the use of ultrasound and magnetic resonance imaging, but around half of respondents advocated combining the HJHS with measures of physical function and quality of life. Despite the growing number of instruments such as the Haemophilia Activities List (HAL) and PedHAL [18, 19, 20, 21], the HaemoQoL and HaemAQoL [22,23] and Hep-Test-Q [24], they do not appear to be widely used in clinical practice. While 25% of respondents indicated that the PedHAL and HAL were routinely used, no physiotherapists were aware of the HaemoQoL, HaemAQoL or Hep-Test-Q being used.
Discussion
The physiotherapists who completed the survey represented most comprehensive care centres across the UK as well as some of the larger non-comprehensive care centres, suggesting that the survey is representative of practice across the country for adults and children. It is of concern that almost half of all of respondents were allocated to haemophilia for just 1 or 2 days each week, even though all of the centres represented would have at least 40 severe haemophilia patients [25]. Nearly all respondents were doing joint scoring using the HJHS (83%), from both adult and paediatric centres, and therefore meeting the requirements of healthcare commissioners and the UKHCDO, even though the HJHS was not intended for use in adults.
While it is reassuring that joint scoring was only undertaken by physiotherapists, this probably reflects the fact that the questionnaire was sent only to physiotherapists; it is known that in smaller centres lacking a physiotherapy service, haemophilia nurses or doctors are sometimes expected to perform joint scores. Our respondents overwhelmingly believed that the joint score assessment could not reliably be done by other health care professionals; only physiotherapists were adequately trained in observing the musculoskeletal system and in taking precise measurements of joint function, as well as being able to implement a care plan based on adverse findings in the assessment. It is acknowledged by the authors that this may be a perspective particular to the UK, as physiotherapists are autonomous practitioners, trained to be independent in their assessment and treatment plans. In many other countries in the world this is not the case, and other professionals such as physiatrists, rheumatologists and orthopedists may be responsible for completing the joint assessment. However, all those who use the tool must have been adequately trained and appraised in its use.
It is reassuring that most haemophilia patients are having at least an annual joint assessment, with more frequent assessments being offered to children and adolescents. Patients with mild haemophilia were rarely seen: several physiotherapists commented that they might do a joint assessment as a baseline in a mild haemophilia patient and then only repeat it if problems arose.
The HJHS assessment was originally developed in response to the finding that the WFH Physical Examination (WFH-PE) scale, a measure of joint and muscle impairment, was not sufficiently sensitive to detect the minor joint changes that are often more apparent in children and adults who have had access to factor replacement on a regular basis. The HJHS has been validated only in children [8]. It is not an outcome measure: there is no known relationship between joint score and use of clotting factor in the literature. Nevertheless, it is one of the pieces of data increasingly required by commissioners of care in the UK. The assessment takes around 90 minutes to do. While this can clearly be scheduled into a patient’s regular clinic review, over-reliance on this pro-forma approach to care together with the limited time available in the clinic setting can mean that the physiotherapy assessment becomes little more than a box-ticking exercise in which the physiotherapist focuses only on the elbows, knees and ankles at the expense of the rest of the musculoskeletal system. This is particularly likely to be the case where the physiotherapist has only limited time in haemophilia and a high caseload. While it is an administrative burden, many physiotherapists feel that the joint score can offer the opportunity to develop a close relationship with the patient, and it can highlight unanticipated rehabilitation needs.
In this respect, it is gratifying to see that joint scores are usually recorded in the patients’ clinical notes and generally have a direct bearing on the patients management plan, with changes in the joint score frequently being fed back to patients: comments to the survey suggested that where a clinical situation mandates a change in treatment such as an increase in prophylaxis dose, it should be possible for the physiotherapists to use the score within specific joints to incentivise patients to enhance concordance with treatment and in these specific cases it could be considered an outcome measure of that prophylactic regimen. However, it is important to bear in mind that scores are patient specific and will fluctuate over time as individuals alter their activity profiles and joint damage progresses or improves.
A retrospective case note review study has shown that the HJHS is a useful tool for identifying factors that affect the joint score; these included inhibitor status, age and early or late prophylaxis [10]. Scores are not directly comparable between patients due to the variability of individual patients treatment, medical history and activity levels. Furthermore, the range and magnitude of any change in joint score that might constitute a clinically important difference to patients remains unclear and requires further quantification and determination of functional relevance.
In this survey, most physiotherapists did not feel that the total HJHS score reflected total joint health, principally because it omits the hips and shoulders where assessment is important in older patients. As yet the relationship of the joint score with the patient’s present and future quality of life and functional capacity is unclear although a retrospective analysis has suggested the total joint score correlates with patients’ self-reported perception of function, particularly with respect to the lower limbs [26]. However, while the joint score correlates highly with age, function alone correlates poorly with age [26]: it may be that this is linked with the patient’s past treatment and expectations of what their haemophilia means for them and how they have accommodated to their lifelong physical disablement.
While measures of impairment may be relevant to health care providers in that they assess range of movement, they may be less relevant to affected individuals who are more interested in their ability to undertake functional activities. Our survey found that only a minority of centres routinely used measures of self-reported physical function. One quarter of centres routinely used the HAL or PedHAL but none routinely used the Hep-Test-Q or
HaemoQoL/HaemAQoL. Such patient-reported outcome measures have an increasingly accepted role in assessing the quality of care delivered to patients from the patient perspective [27] and are frequently used in clinical trials and observational research studies. Anecdotal reports suggest that commissioners of health care are increasingly requiring haemophilia treaters to use them in order to justify the use of high dose and/or intensive prophylaxis. However, it remains unclear whether these scores add to the data already routinely collected in haemophilia care and indeed whether they are acceptable to patients.
Furthermore, those questionnaires that focus on the assessment of perceived functional ability (such as the HAL and PedHAL) may not be fully appropriate for children and teenagers who have benefited from prophylaxis and who do not consider themselves to be “physically impaired”. The planned Study Of physical Function In adolescenTs with haemophilia (SO-FIT) will seek to explore the correlation between joint scores and self-perceived functional ability and quality of life in children and young people with severe haemophilia [28]. The study also aims to assess the acceptability of currently available functional outcome scales and whether or not completion rates can be enhanced by the use of mobile devices in the clinic rather than pen and paper.
This survey has shown that most UK physiotherapists complete joint scores on adults and children with moderate and severe haemophilia. Most physiotherapists expressed the opinion that joint scores did assist patient care, but a battery of assessments may be required to complement the joint score. To date it remains unclear what the functional relevance is of the joint score to the patient or to disease progression. Data from these assessments should be collected longitudinally to establish any clinical relevance
Conclusion
The findings of this survey suggest that future physiotherapy practice should continue to collect joint scores for individual disease monitoring. The use of joint scores requires continued standardisation across the UK if the data is to be used in clinical research. It is a positive development to see that joint scores are being widely used in clinical practice. However, physiotherapy is and must remain more than a means of collecting joint scores. Furthermore, it remains unclear how useful these measures are in the adult population. Future clinical assessments and research should consider more joint specific outcome tools to identify any correlation between joint scores and function. The UK is ahead of the rest of the world in attempting to gather joint score data, however this needs to remain within the domain of specialist physiotherapists who can use the joint scores as part of their assessment battery of patients and ultimately improve the musculoskeletal health of patients.