A roundtable of UK experts representing different specialities within the haemophilia multidisciplinary team (MDT) suggest that haemophilia management incorporating both face-to-face and virtual consultation will facilitate the optimisation of MDT care

Haemophilia is a rare inherited bleeding disorder that impacts the blood’s ability to clot due to reduced levels of blood-clotting proteins. This can lead to spontaneous bleeding as well as prolonged and excessive bleeding following injuries or surgery [1]. The haemophilia patient journey can be complex, involving various procedures, treatments and multidisciplinary specialities [2]. Factor replacement products are the mainstay of treatment; however, monoclonal antibody therapies provide an alternative non-factor treatment option, with one product licensed for prophylactic use in appropriate patients with haemophilia A via subcutaneous administration [3–6]. Recently, the development of haemophilia gene therapies has progressed significantly, with one product approved for the treatment of suitable adults with severe haemophilia A and another product approved for the treatment of suitable adults with haemophilia B [7–12]. These significant treatment advances together with the multiple heterogeneous therapy options available have added complexity to treatment selection and necessitates a collaborative approach [13].
As well as preventing and controlling bleeding, care for people with haemophilia includes management of pain, musculoskeletal complications, and other comorbidities, and monitoring/managing clotting factor inhibitors [3,4]. In addition to controlling physical symptoms, psychosocial care is also of high importance [3]. There is an overriding need to ensure minimal impairment of quality of life, and the importance of minimising the psychological burden has been recognised [14]. These broad needs are best met by a multidisciplinary team (MDT), where treatment decisions are made jointly with the patient and their caregiver(s) [3]. The practicalities of this have been greatly affected by the coronavirus disease 2019 (COVID-19) pandemic [15].
Many healthcare settings have adopted virtual telemedicine approaches [16], however, there is limited guidance on how to successfully integrate this approach into MDT haemophilia care. Considering published literature and expert opinions, this publication aims to understand the current landscape of MDT haemophilia care, focusing on a virtual approach and how this may evolve in the future.
METHODS
Literature review
A literature review was conducted by a medical communications agency prior to a roundtable meeting with experts from the United Kingdom (UK), to facilitate relevant and current discussions. Searches were performed in PubMed in June 2021 using the following search strings: Hemophilia AND (Telemedicine OR Telehealth OR Teleconsultation OR Virtual) and Hemophilia AND (Multidisciplinary OR Comprehensive OR Team) AND (COVID-19). The search results underwent an initial title/abstract screen by the first reviewer. The same reviewer then reviewed the full text of these publications and selected those of relevance. A second reviewer verified the relevance of these selected publications. Publications were excluded if they did not provide detailed information on multidisciplinary care during the COVID-19 pandemic and/or virtual care, or primarily focused on treatment endpoints, instead of the model of care. Additional relevant literature published following the initial search (between June 2021 and September 2022) was also included to ensure the latest research was captured. The process used for the initial literature search was also used to identify this additional relevant literature; the search strings used within PubMed can be found in Supplementary Table 1. Publications were excluded if they related to acquired haemophilia or specifically to pain management.
Table 1.
Best practices for haemophilia care, based on a survey of healthcare professionals in the United Kingdom and Canada [21]
1 Adapted from St-Louis J, Chowdary P, Dolan G, et al. Multidisciplinary team care of patients with hemophilic arthropathy: A qualitative assessment of contemporary practice in the UK and Canada : Canada/UK: MDT Practices for Hemophilia. Clin Appl Thromb Hemost (SAGE) 2022; 28. doi: 10.1177/1076029621107002. Licensed under CC BY-NC 4.0: https://creativecommons.org/licenses/by-nc/4.0/. © The Author(s) 2022.
Roundtable meeting
In the summer of 2021, eight representatives of the specialities involved in MDT haemophilia care, from various UK-based haemophilia comprehensive care centres (HCCCs), were brought together by CSL Behring. The group (current authors) comprised four haematologists, a psychologist, two physiotherapists and an advanced nurse practitioner. The roundtable meeting was held virtually on 29 September 2021 and involved presentations on predefined topics (based on findings from the literature review and the participants’ own experiences) and group discussions, with the aim of addressing the following objectives:
Understand the current landscape of MDT care for haemophilia and best practices for delivering effective care
Assess the benefits, challenges and opportunities of virtual MDT care
Discuss how bleeds are identified and managed in a virtual setting
Explore how virtual paediatric care differs from adult care
Discuss the future of virtual MDT care.
The outcomes from the roundtable meeting are presented, along with additional points voiced during the development of the manuscript. These findings were summarised to form consensus statements, which were reviewed and approved by all authors.
RESULTS
Literature review
The initial literature review and additional literature searches produced a total of 1,112 results. Following removal of duplicates and review by the agency, 68 publications were identified as relevant and detailed the delivery of virtual and/or multidisciplinary haemophilia care (Supplementary Tables 2 and 3).
The current landscape and best practices for effective MDT haemophilia care
Literature findings
International guidelines recommend that comprehensive haemophilia care should be delivered by a MDT, usually consisting of a haematologist, nurse, psychologist, laboratory specialist and physiotherapist [3,17–20]. In the United States (US), the addition of a clinical haemophilia pharmacist to the MDT was associated with a reduction in bleeding rates and medication costs [20].
Several best practices for haemophilia care, including MDT care, have been identified by healthcare professionals (HCPs) in the UK and Canada (Table 1), which involve a non-hierarchical team attitude and regular meetings [21]. In the US, haemophilia treatment centres (HTCs), specifically designed to provide multidisciplinary care, have received high levels of patient satisfaction and have been associated with fewer bleeds and associated emergency department visits, as well as a positive impact on patients’ quality of life [22]. Tools and algorithms are also in development to improve MDT care and assist with shared patient and provider decision-making in the current landscape of multiple diverse therapy options [13].
The necessity of MDT care is well recognised globally [3]; however, there are still several associated unmet needs associated, such as pain management, improved access to HTCs and involvement of additional specialities during HTC visits [23,24]. Moreover, priorities in resource-limited countries differ from those in rich countries. The importance of medication access and the potential challenges associated with adherence have been the focus of literature from these regions [25,26].
Prior to the COVID-19 pandemic, virtual MDT haemophilia care was gaining support worldwide [27–29]; however data was limited [15]. The pandemic necessitated rapid implementation of innovative virtual solutions to ensure continued access to multidisciplinary care [15]. In the US, the use of telemedicine showed a 78-fold increase between February and April 2020. Despite a subsequent decrease, a 38-fold increase versus the pre-pandemic level was still evident in February 2021 [16]. During the pandemic, paediatric care remained accessible to patients but in adapted forms (e.g., via telemedicine) across HTCs in Europe, Israel and Canada [30]. A European survey completed in 2021 reported that virtual pharmacokinetic tools were being utilised by many centres [31]. One mobile application in development for patients with haemophilia features medication reminders, remote communication with healthcare providers and self-monitoring logs, with the aim of aiding self-management [32]; however, data privacy and the patient’s willingness/ability to use technology require further consideration [33].
Roundtable discussions
In the UK, virtual MDT care was widely used throughout the pandemic; however, the format varied depending on the healthcare setting and available resources. A mix of video software/platforms, including Microsoft Teams, Attend Anywhere, Zoom, Skype, accuRx and WhatsApp, were used prior to and during the pandemic, with the choice of platform depending on HCP and MDT preferences and local policy. Following a reduction in COVID-19 rates, hybrid care formats were being adopted in most settings, enabling greater flexibility in the delivery and personalisation of care.
Virtual MDT care – benefits, challenges, and opportunities
Literature findings
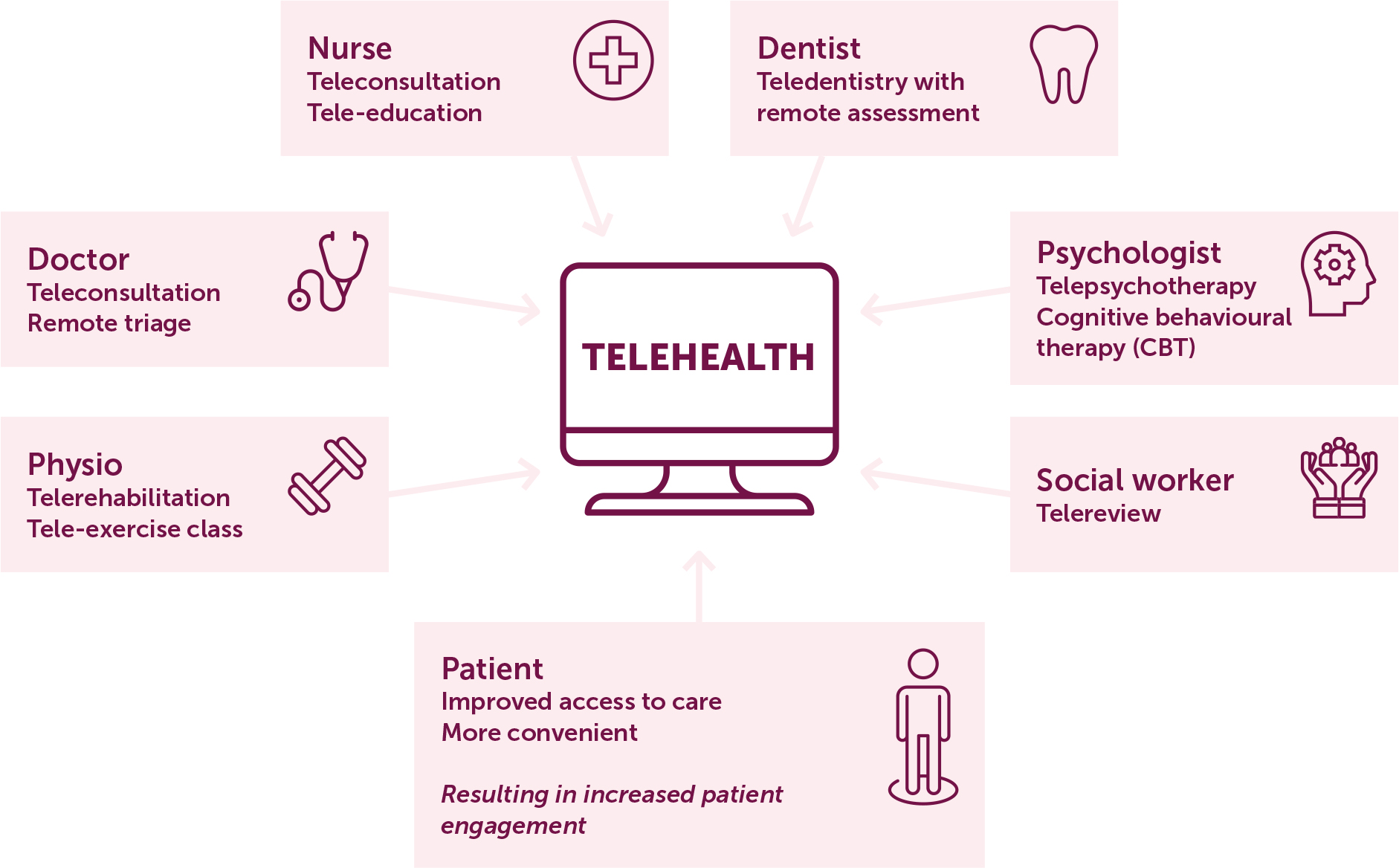
Several studies have described the benefits associated with virtual MDT care. Implementation of a multidisciplinary approach using a virtual platform at a HCCC in Belfast, UK, was positively viewed by patients and staff and was associated with higher attendance rates (93% virtual versus 69% face-to-face clinics) [34]. In Dublin, Ireland, the use of telehealth for the delivery of comprehensive care (e.g., medical, nursing and physiotherapy appointments) (Figure 1) increased the number of patients undergoing consultations and reduced non-attendance rates compared to the previous year [15].
Figure 1.
Telehealth care model for haemophilia care, implemented during the coronavirus disease 2019 (COVID-19) pandemic at a haemophilia comprehensive care centre in Dublin, Ireland [15]
From: O’Donovan M, Buckley C, Benson J, et al. Telehealth for delivery of haemophilia comprehensive care during the COVID-19 pandemic. Haemophilia (Wiley) 2020; 26(6): 984-990. doi: 10.1111/hae.14156. © 2020 John Wiley & Sons Ltd.
The challenges of virtual haemophilia care have been particularly described for physiotherapy and rehabilitation [35]. Although telehealth may be applicable to some aspects of this care (e.g., triaging for acute concerns), some face-to-face contact is expected to remain necessary [36]. When assessing patients, physical examination is an important tool and both physiotherapists and patients have expressed concerns that this is not possible in a virtual setting [35,36]. In addition, patients may not own the correct equipment to adequately benefit from the virtual session [35]. Assessment tools, such as the Haemophilia Joint Health Score, intended for in-person consultations, require adaptation for remote use [36]. While newer products may provide improvements in treatment effectiveness, the need for physiotherapy is expected to persist and services will need to evolve as the landscape progresses [37].
Further challenges of virtual consultations include the lack of deep discussion and disclosure of private information [34]. The inability to carry out physical examinations or specific testing may lead to further face-to-face appointments [34]. In addition, video consultations require access by both patients and HCPs to appropriate IT equipment, and organisational processes may require adjustments to avoid dependence on physical presence [15].
Roundtable discussions
The advisors agreed that virtual MDT care is associated with several benefits, which include improved convenience and choice for their patients, as well as access to a wider network of patients. However, there are also many patient-specific challenges, such as difficulties building relationships and gaining the trust of new or newly diagnosed patients, and complexities with gaining a thorough understanding of the patient’s needs. For paediatric patients, ensuring sufficient engagement and safeguarding, and that parents/guardians are present throughout the appointment, can be challenging. Furthermore, in virtual settings, indicators of abuse/neglect may be less recognisable.
Logistical difficulties, such as space limitations and ensuring privacy from other household members, may be encountered when evaluating patients virtually. In particular, joint and musculoskeletal assessments may be restricted, due to only being able to observe instead of assessing hands-on. Consultations overrunning or taking longer, inappropriate appointment locations (e.g., whilst driving) and technical issues may also present problems. From the perspective of the healthcare system, students and trainees may not get the opportunity to undertake placements and practical learning experiences. Opportunities to optimise virtual care include the development of new hybrid care models and interactive virtual materials, plus increased use of administrative staff to organise hybrid care, including checking-in patients and confirming key information prior to virtual appointments.
Consensus statement
Advisors agreed that virtual MDT care is associated with several benefits such as improved convenience/choice for their patients and wider patient reach; however, many patient-specific and logistical challenges exist and require attention. Hybrid care models may provide an opportunity to overcome these challenges and further optimise MDT care.
Managing bleeds remotely
Literature findings
The World Federation of Hemophilia (WFH) recommends that patients are taught how to manage their care at home, empowering them to recognise bleeds and to self-infuse. Self-management promotes rapid treatment, minimising the effects of bleeding. Ability to recognise and treat breakthrough bleeding is important for patients receiving prophylaxis with new types of coagulation therapy, and this capability should be assessed by their physician [3].
Patients should keep detailed records of treatments administered and bleeding episodes experienced [3]. It has been demonstrated that electronic diaries may be associated with more comprehensive data reporting, as well as an improvement in treatment adherence [38]. In the UK, Haemtrack is an established and widely used system for patients with bleeding disorders [39]. Although paper versions are available, the majority of patients opt to use the electronic diary, accessible via PC software and mobile applications [39]. HaemoassistTM 2 is another system, predominantly used in Spain and Germany, shown to be effective in enabling patients to document their prophylactic infusions and treatment of bleeding [40]. A study in Hong Kong reported that patients are receptive to using mobile technology to organise their bleeding records and manage their health [41].
Roundtable discussions
The care model for bleeding management varied among advisors. Some advisors prefer for patients to have a face-to-face assessment for acute bleeding and a virtual follow-up, while others prefer to assess remotely so the patient can rest, with a face-to-face follow-up after rehabilitation. Telephone consultations alone are not sufficient for assessing bleeds as it is not possible to identify non-verbal cues and movement restrictions. Advisors are more comfortable with assessing bleeds remotely in patients with whom they have strong and trusted relationships, enabling confidence in the patient’s ability to self-manage. Face-to-face assessments are preferable for new and newly diagnosed patients, patients with mild/moderate disease and those known to require ongoing support. The group agreed that patients should be assessed in person if there is any uncertainty surrounding the bleed.
It is important to encourage frequent and open dialogue with patients who are self-managing remotely. A bleeding episode described by a patient may not represent the overall clinical situation and may require further assessment. Virtual tracking tools (e.g., Haemtrack) are used in some centres to manage patients remotely and, while usage increased at the beginning of the pandemic, it has subsequently declined. Hesitancy among HCPs to rely on virtual tracking tools may be attributable to the risk that patients may not document their bleeds in an accurate or timely manner. The use of home delivery of medication was described by one advisor; their centre first implemented this during the pandemic and a positive reception was received.
Consensus statement
The decision as to whether bleeds are managed virtually or face-to-face should depend on provider preference, the patient-provider relationship, and the patient’s disease severity, history, and ability to self-manage. As such, this should be assessed on a case-by-case basis. Virtual tracking tools should not be solely relied upon for MDT decision-making as patient accuracy cannot be ascertained.
Adapting and optimising virtual paediatric care
Literature findings
No published literature reporting experiences of virtual paediatric care were found. Home therapy for children with haemophilia is advocated by the WFH [3]. For young children, family and carers may be trained to administer coagulation factor concentrates, while older children and teenagers can be taught self-infusion. The need for education is high; children must understand more about their condition as they become older and seek to gain the skills required for self-care [3]. It is important to note that educational activities may require adjustment according to each child’s health literacy and health numeracy [42]. Equally, the educational needs of parents must not be overlooked. It has been reported that parents want to be taught how to administer intravenous treatment and how to prevent/treat injuries [43].
Adherence to treatment among adolescents can be suboptimal, for reasons such as low burden of symptoms, forgetfulness, and poor knowledge of the disorder, as well as challenges with self-infusing. Young adults may feel pressure to appear normal and may be in denial about their condition [3,44]. Intravenous prophylaxis may also present challenges in the younger population; the potential option for subcutaneous administration could reduce the treatment burden but may also decrease the ability to self-infuse due to lack of venepuncture training [45].
Roundtable discussions
Paediatric patients are as likely as adults to benefit from a virtual MDT approach; however, the composition of an ideal MDT may differ from that of adults and care must be taken to ensure that both patients and their caregivers receive appropriate support and communication to facilitate suitable virtual care.
Transitioning adolescent patients to adult clinics without face-to-face consultation is challenging, partly due to difficulties in building relationships when interacting virtually. It is important to start the prolonged transition process of these patients early, avoiding uncertainty in which service is responsible for their care and allowing a gradual increase in independence as they leave the paediatric clinic. Transition clinics should be adapted to the needs of patients and their parents and enhanced psychological support may be needed during the adjustment period. Patients may benefit from a hybrid care approach. One advisor described an adult transition clinic at their centre which runs into the evening, thereby minimising the amount of school that teenagers are missing due to clinic appointments.
It is difficult to train patients/parents to administer prophylactic treatment and provide support/reassurance virtually, particularly for newly diagnosed patients. Virtual care has facilitated increased use of creative platforms (e.g., YouTube, Instagram, TikTok) to educate and communicate with younger patients. Interactive and digital materials may help increase engagement among patients and their parents, particularly for those with mild disease who do not require regular appointments. Some suggestions for materials included virtual clinic tours, online biographies about their care providers, and digital leaflets.
Consensus statement
The MDT composition for paediatric care should be tailored to the specific needs of the age groups and their parents/caregivers. Creative virtual platforms and interactive materials may assist with engaging and educating this population, whilst also providing support to patients and their family support system.
The future of virtual MDT care
Roundtable discussions
Hybrid, integrated MDT care, delivered via specialist treatment centres, is likely to remain the gold standard for haemophilia care. Virtual MDT care was exciting, novel and a necessity at the start of the pandemic but now there is virtual fatigue and a need to increase the availability of face-to-face care. The method of care delivery should be individualised to the patient, based on their preference, patient-provider relationship, and disease severity. One advisor voiced that paediatric patients with mild haemophilia can be seen virtually, but it is still important to have face-to-face appointments at an appropriate interval; children with severe haemophilia should be seen face-to-face every six months. Another advisor described how their centre sees adult patients with severe haemophilia once in person each year for a full musculoskeletal and medical review, and once virtually each year, with high patient satisfaction. Some elements of haemophilia care, such as musculoskeletal and joint health assessments and laboratory monitoring, cannot be satisfied virtually. Face-to-face connections will remain valuable for conducting physical assessments, building strong relationships, and enabling HCPs to provide patients with reassurance, understanding and support. Hybrid care models with an adaptable mixture of face-to-face and virtual appointments will help provide flexible and individualised care in the rapidly evolving haemophilia landscape.
CONCLUSIONS
MDT care is widely recognised as the optimal approach for haemophilia management. The COVID-19 pandemic triggered a rapid uptake of telehealth for healthcare provision, which led to higher attendance rates in some centres, as well as important perceived advantages such as improved convenience for patients and wider patient reach. However, some aspects of face-to-face consultations (e.g., musculoskeletal and joint health assessments) cannot be replicated virtually; one comprehensive review found no articles describing how virtual assessments were performed in haemophilia [46]. Future research should focus on the standardisation, validity and reliability of virtual assessments in haemophilia, as well as the patient perspective of the methods, benefits and challenges of virtual MDT care. Hybridised care with both face-to-face and virtual options depending on patient preference, clinical circumstance, and patient-provider relationship, will likely be adopted for future haemophilia management and will facilitate the optimisation of MDT care.