A study among PwH attending a clinic in Assam, India, recommends combining clinical and radiological tools (e.g. using HJHS and FISH with HEAD-US) as a cheap and reliable option for assessing joint health consistently in resource-constrained settings

Haemophilia is an X-linked inherited bleeding disorder characterised by an absence or deficiency of Factor VIII (FVIII) in haemophilia A and Factor IX (FIX) in haemophilia B. It principally affects males, although lyonization may result in females having haemophilia [1,2] and women who carry the haemophilia gene may experience bleeding symptoms [3]. Females may also have haemophilia as the result of a consanguineous relationship where the mother carries the haemophilia gene and the father has haemophilia [4]. Sporadic mutation occurs in almost 30% of cases, without any suggestive family history [5]. The prevalence of haemophilia A (all severities) is 17.1 cases per 100,000 males; for haemophilia B (all severities) it is 3.8 cases per 100,000 males [6,7]. According to the most recent data published by the World Federation of Hemophilia (WFH), there are 209,614 identified cases of haemophilia globally (165,379 haemophilia A; 33,076 haemophilia B; 11,159 haemophilia type unknown) [7]. In India, which has a population of over 1,380,0000, the WFH reported 22,594 people registered with haemophilia A and 743 with haemophilia B in 2020 [7]. These numbers are known to be highly underestimated and it is thought that the true figure could be up to 100,000 [8]. As such, despite being a low public health priority historically, this is now starting to become a public health concern [9].
Haemophilia has a spectrum of clinical manifestation, ranging from easy bruising and gum bleeding to haemarthrosis (bleeding into the joint) and intra cerebral haemorrhage. Disease severity is the strongest predictor to clinical manifestation, but bleeding phenotype is also important. Within a haemophilia population with a severe genotype, there is a large variability in annual bleed rate (ABR) [10]. Haemarthrosis is a common manifestation of haemophilia and is the most common risk factor for development of haemophilic arthropathy (HA), a crippling joint disease which can result in severe disability and a need for joint replacement [11,12]. Despite the availability of factor replacement therapy, including prophylaxis, to treat and prevent bleeding, arthropathy continues to be the most common complication of haemophilia and significantly impairs quality of life in people with haemophilia (PwH) [13,14].
Regular, periodic assessment of joint status in haemophilia patients has been recommended to identify early arthropathic changes and prevent the development or progression of haemophilic arthropathy [15]. Alongside clinical examination of the joint, a number of modalities have been developed for the assessment of joints in haemophilia, both clinically and radiographically. For the functional assessment of joint modalities, haemophilia-specific tools such as the Hemophilia Joint Health Score (HJHS 2.1) [16,17] and Functional Independent Score in Hemophilia (FISH) [18] are helpful. Though kinematic and kinetic assessment are preferable, their availability is limited in developing countries; HJHS scoring is widely used due to its high sensitivity and excellent inter-rater and intra-rater reliability. Radiologically, magnetic resonance imaging (MRI), as the most sensitive measure of joint structure, is the gold standard for diagnosing haemophilic arthropathy and is able to show early soft tissue and osteochondrial changes [17]. However, as well as there being difficulties in using MRI with children, it is expensive and there is limited availability in resource-constrained settings. Ultrasound is effective in assessing changes to soft tissue and cartilage in early arthropathy [16,17] and its use with the HEAD-US scoring system has shown similar sensitivity [19]. X-rays are not sensitive enough to detect early arthropathy but can show changes in the later stages when arthropathy is already established. Use of Pettersson scoring is therefore not so helpful in detecting early changes [15,20].
There is a known shortage of imaging equipment in low- and middle-income countries – in many Asian and sub-Saharan African countries, access to MRI scanners has been estimated at one per million people [21]. However, it remains important to identify the biomechanical changes that indicate early arthropathy to ensure that it is diagnosed in a timely way and that PwH affected have appropriate treatment. This study, conducted among people with PwH treated at Assam Medical College and Hospital in Northeast India, is designed to identify which radiological assessment tool(s) work best when integrated with clinical assessment tools to examine joint health in PwH, with the aim of establishing a cheap, effective, multimodal approach to joint assessment in clinical practice in low resource settings which can then help to guide treatment.
METHODS
A cross-sectional study was carried out among PwH attending a clinic in the department of medicine at Assam Medical College and Hospital, Dibrugarh, Northeast India, over a one-year time period from 1 June 2019 to 31 May 2020. The elbow, knee and ankle joints of eligible participants were assessed clinically and functionally using the HJHS and FISH scoring systems and radiologically by the Pettersson (X-ray) and HEAD-US (ultrasound) scoring systems. The assessment was undertaken during a single visit by doctors and physiotherapists trained in using these tools. Single blinding was not done. For study participants who presented with acute bleeding, joint assessment was undertaken after the bleeding episode had subsided.
Inclusion criteria
PwH who were clinically diagnosed, confirmed by investigation to have mild, moderate or severe haemophilia A or B, and over 12 years of age were eligible to participate in the study. Patients with other coagulation disorders, those with other diseases affecting joints and taking anticoagulant drugs, those not willing to give consent, and those diagnosed as having chronic liver disease were not included in the study.
Ethics
The study was approved by the Ethics Committee of Assam Medical College and Hospital, Dibrugarh. Consent was taken from each patient or their parent/guardian before enrolling in the study. The objective of the study was explained to each patient or their parent/guardian, and confidentiality of identity was assured.
Data collection
Participants were assessed using a questionnaire. Data was captured on haemophilia severity, type, family history, history of factor usage, and treatment regimen (prophylaxis or on-demand therapy). Detailed data was obtained based on physical examination. Data on annual bleeding rate (ABR), annual joint bleeding rate (AJBR), annual target joint bleed rate (ATJBR), and HJHS, FISH, HEAD-US and Pettersson score were collected.
Statistical methods
Discrete data including ABR, age, FISH, HJHS, HEAD-US and Pettersson scores were expressed as a number and statistical analysis among these variables analysed using the Chi-squared test. Results on continuous data including mean HJHS, FISH, HEAD-US and Pettersson scores were presented as mean ± standard deviation (SD), and comparison was undertaken between mild, moderate and severe groups using Analysis of Variance (ANOVA). Where the p-value was found to be significant (p<0.05) among the three groups, post hoc analysis was used to determine the significance between two individual groups. Statistical analysis for these continuous data was performed using the Statistical Package for Social Sciences (SPSS for Windows, version 21.0. Chicago, SPSS Inc.) and Microsoft Excel 2010. Pearson's correlation coefficient (r) was used to measure the associations among continuous variables. For all analyses, the statistical coefficient was fixed at 5% (p<0.05).
RESULTS
Sixty-seven PwH were enrolled in the study (Table 1). The majority (31/67; 46.27%) were aged 12–19 years, followed by 37.31% aged 20–29 years. The mean age of presentation was 21.69±8.24 (median 21 years).
Table 1.
Participant demographics (n=67)
| NUMBER (N) | PERCENTAGE (%) | |
|---|---|---|
| Age | ||
| 12–19 | 31 | 46.27% |
| 20–29 | 25 | 37.31% |
| 30–39 | 8 | 11.94% |
| 40–49 | 3 | 4.48% |
| >50 | 0 | 0 |
| Gender | ||
| Male | 65 | 97.01% |
| Female | 2 | 2.99% |
| Haemophilia type | ||
| Haemophilia A | 57 | 85.07% |
| Haemophilia B | 9 | 13.43% |
| Acquired haemophilia | 1 | 1.49% |
| Haemophilia severity* | ||
| Severe | 38 | 56.72% |
| Haemophilia A | 32 | 47.76% |
| Haemophilia B | 6 | 8.96% |
| Moderate | 11 | 16.42% |
| Haemophilia A | 9 | 13.43% |
| Haemophilia B | 2 | 2.99% |
| Mild | 17 | 25.37% |
| Haemophilia A | 16 | 23.88% |
| Haemophilia B | 1 | 1.49% |
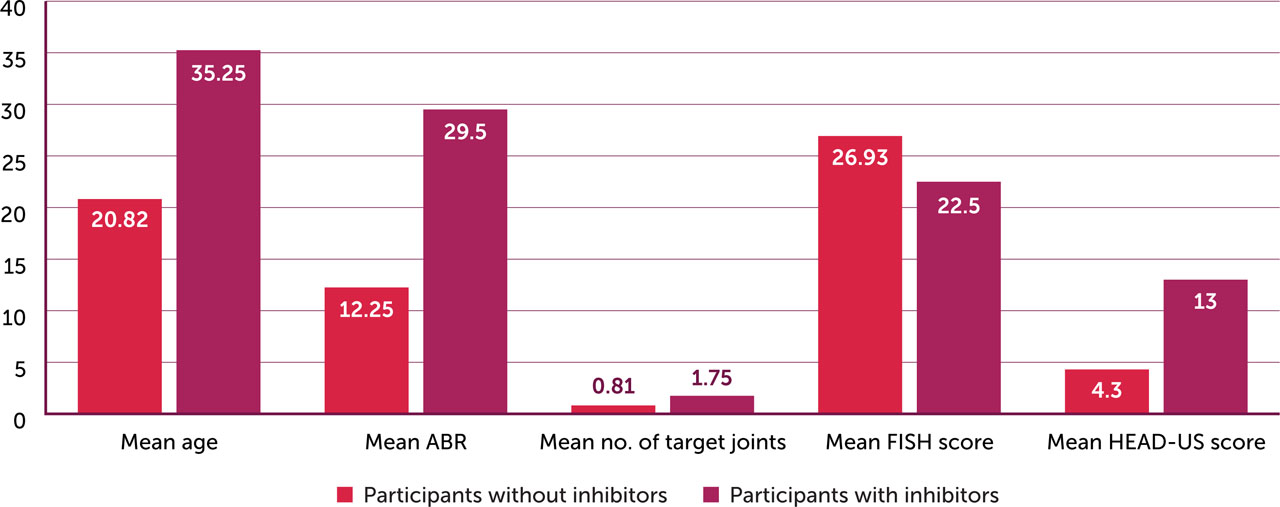
Sixty-five (97.01%) participants were male and two were female. Fifty-seven (85.07%) had haemophilia A and nine (13.43%) had haemophilia B. One participant had acquired haemophilia. Thirty-eight (56.72%) had severe haemophilia, 11 (16.42%) moderate and 17 (25.37%) mild. Four participants had inhibitors. Most (71.70%) presented with joint bleeds, the majority of which involved the knee (82.46%), followed by the elbow (35.09%) and the ankle (22.81%).
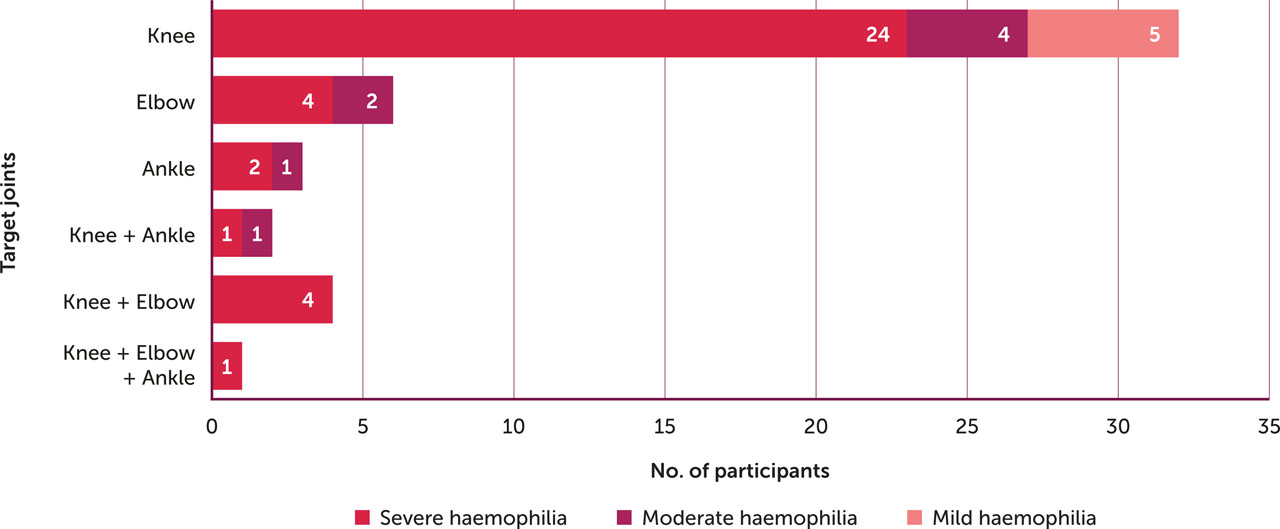
Fifty-seven participants (85.07%) were found to have joint involvement (Figure 1). Among those with affected joints, most (47; 82.46%) had knee joint involvement, 20 (35.09%) had elbow joint involvement, and 13 (22.81%) had ankle joint involvement. The majority (40/57; 70.18%) had the knee as a target joint, followed by the elbow in 11 (19.30%) and the ankle in 6 (10.53%).
Figure 1.
Distribution of target joints in study participants with severe, moderate and mild factor deficiency (n=57)
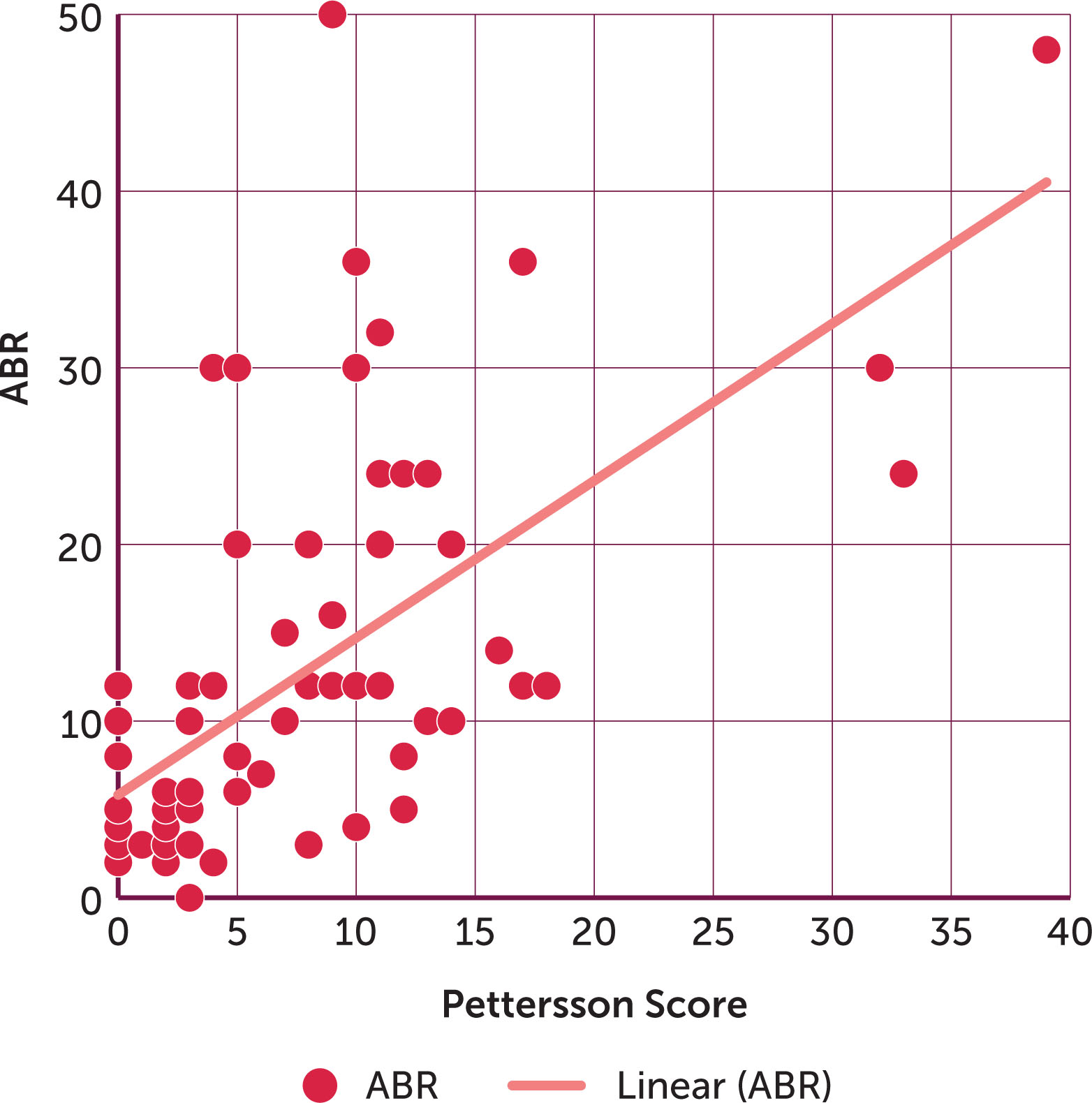
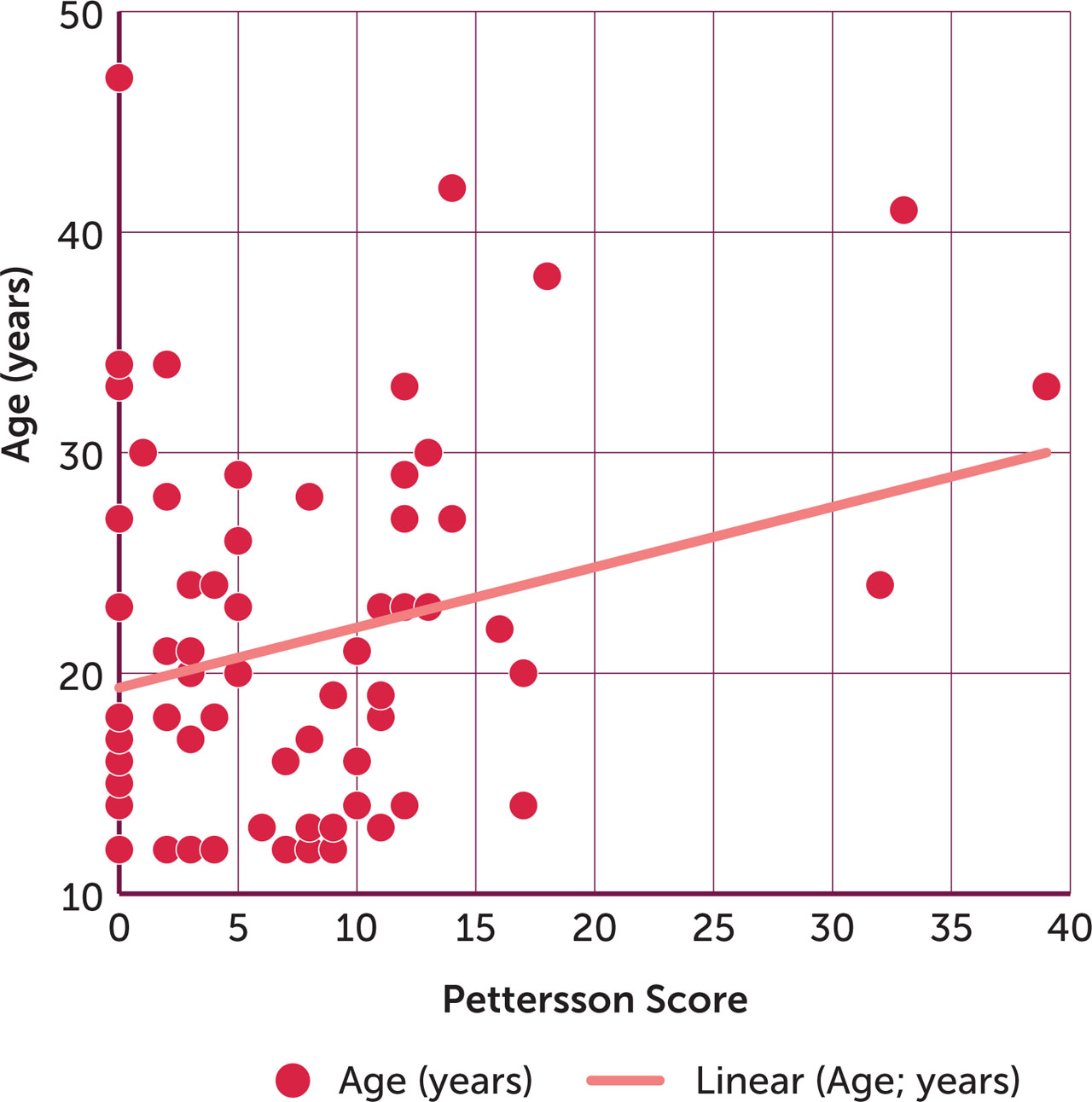
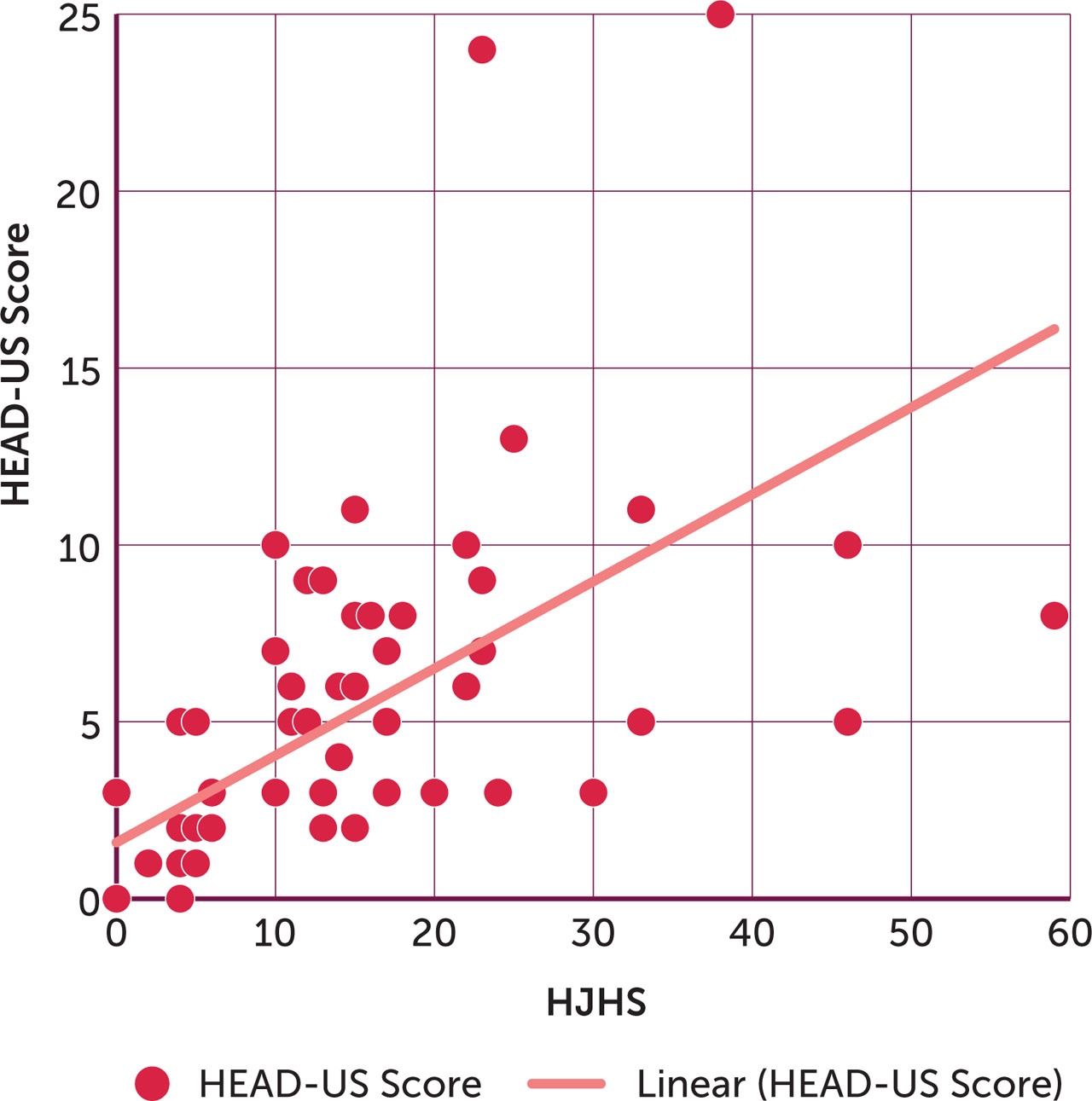
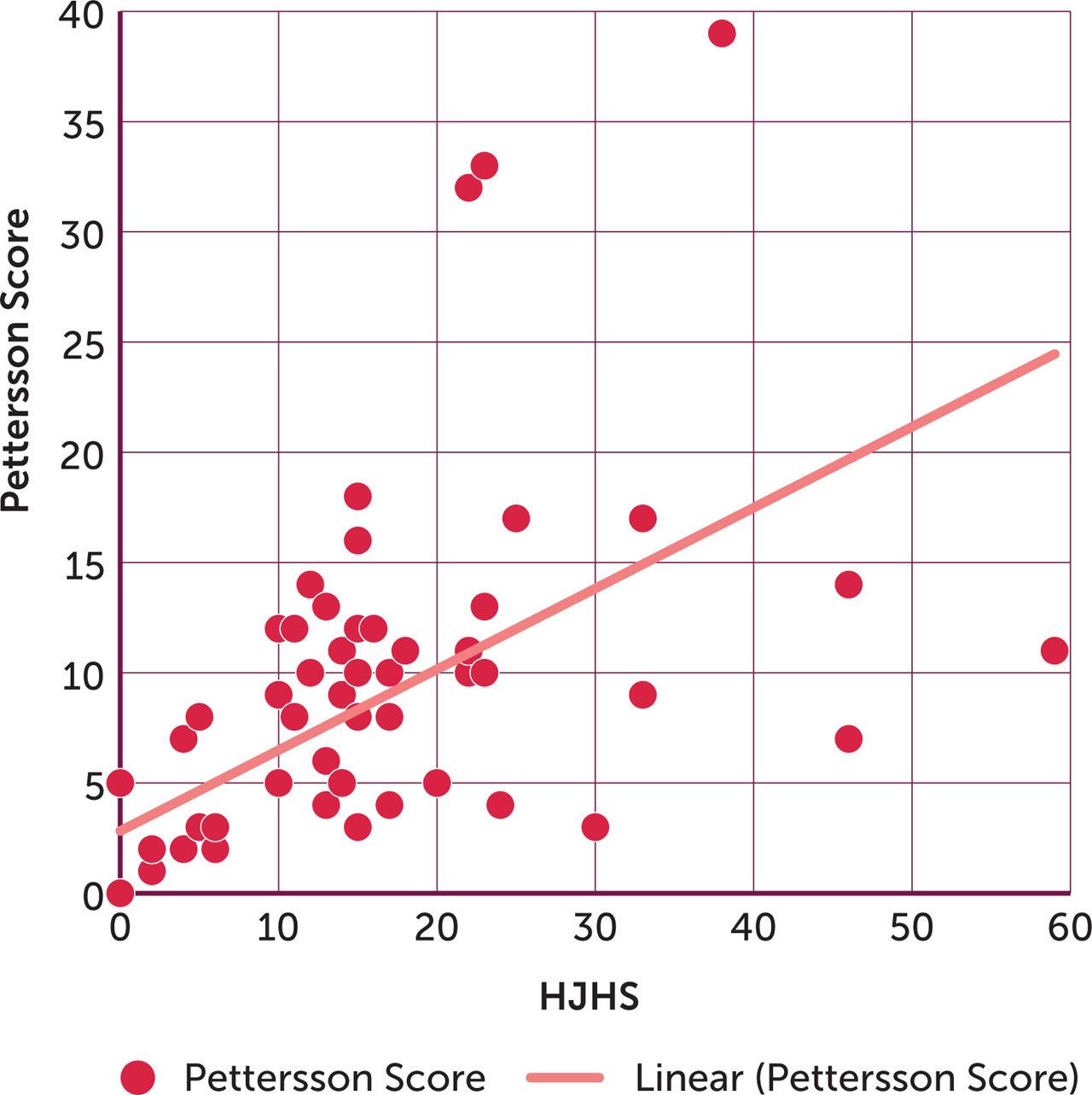
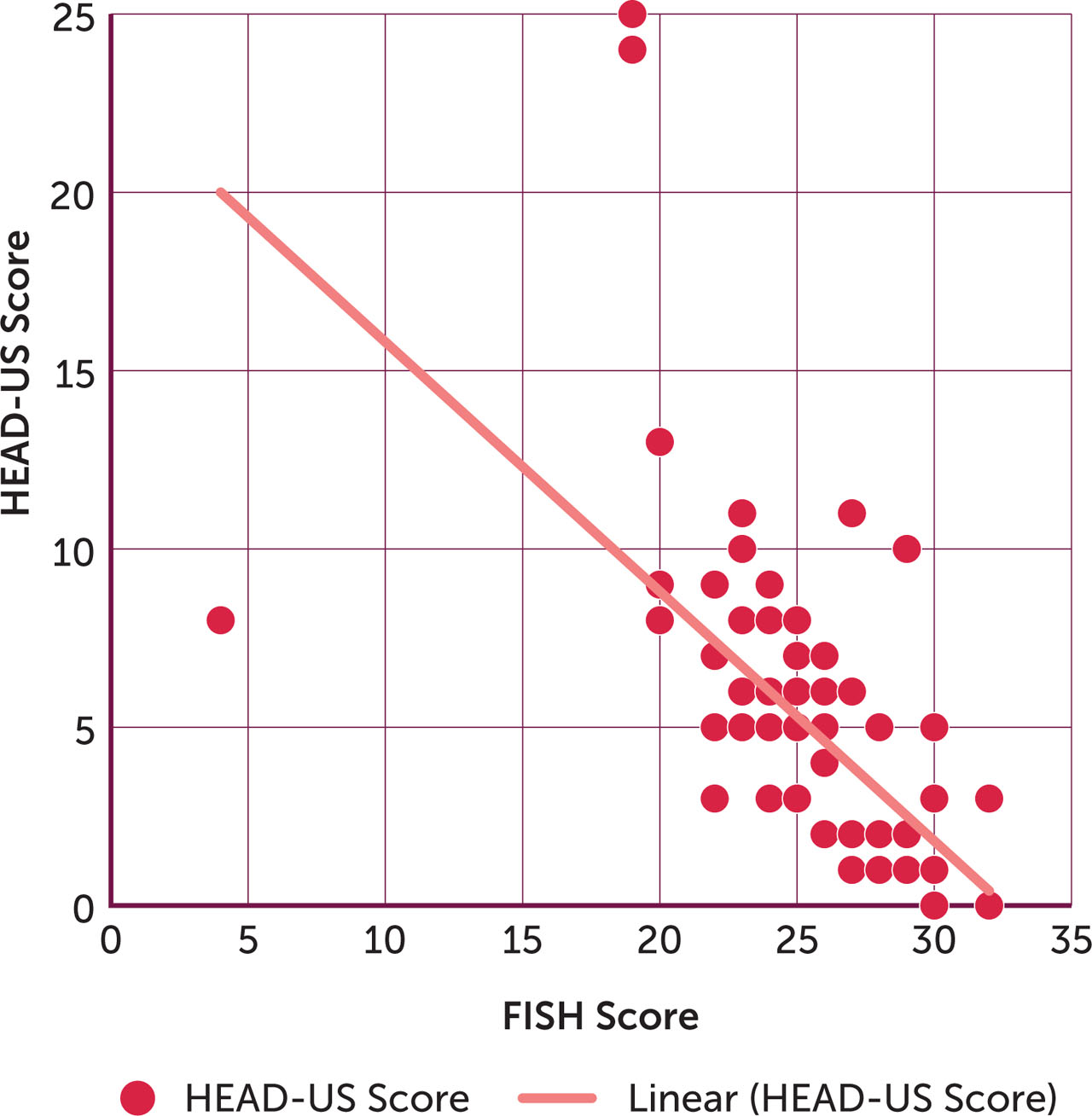
A strong positive correlation was established between ABR (number of bleeds per year) and Pettersson score (r=0.6029, p<0.001) (Figure 2). The correlation between age and Pettersson score (r=0.2531, p< 0.001) (Figure 3) was weak but statistically significant. The degree of association between HJHS score was at maximum with HEAD-US score value (r=0.6062, p<0.001) (Figure 4). There was a statistically significant positive correlation between HJHS and Pettersson scores (r=0.5774, p < 0.001) (Figure 5).
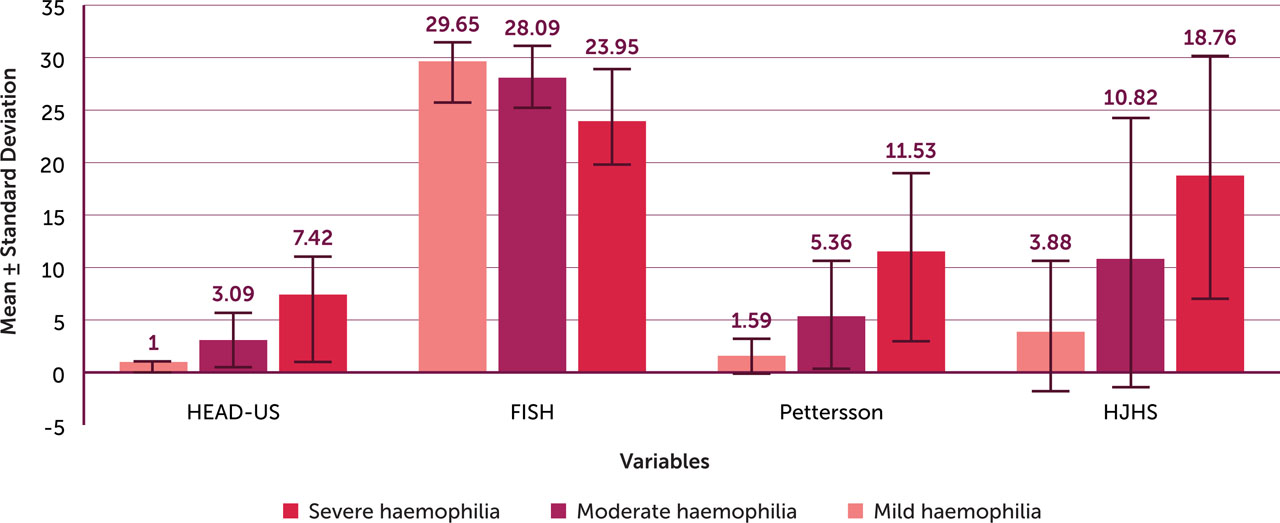
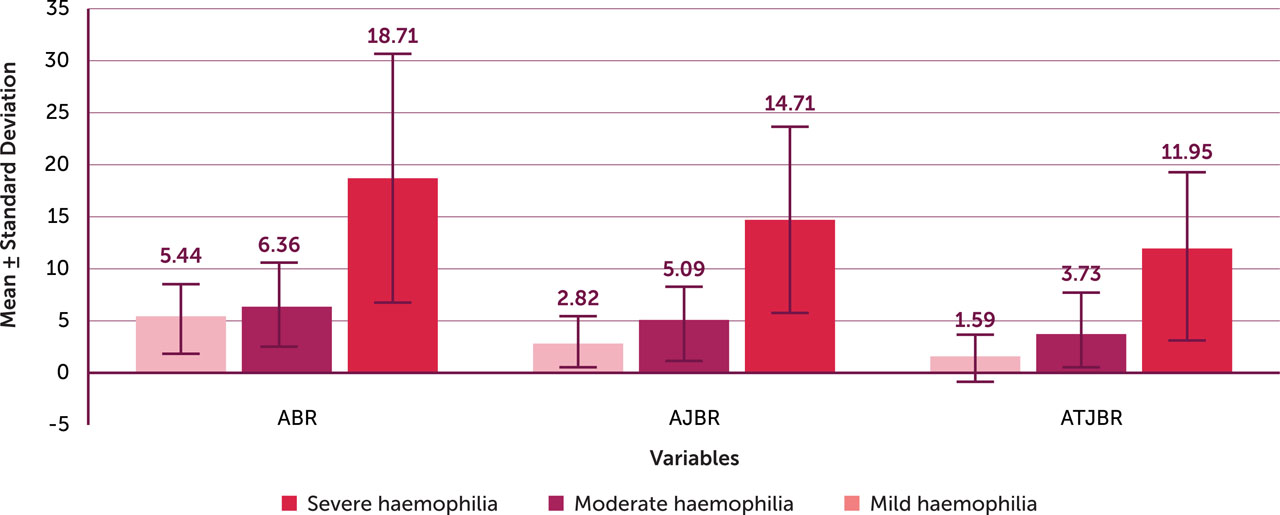
A strong negative correlation was established between FISH and HEAD-US scores (r=−0.6455, p<0.001) (Figure 6). Higher mean HEAD-US (7.42±5.02; median 6.50), Pettersson score (11.53±8.01; median 10.50) and HJHS scores (18.76±11.57; median 16.00) and lower mean FISH score (23.95±4.55; media 24.00) were found in patients with severe haemophilia (Table 2; Figure 7). As shown in Figure 8, the mean value of ABR, AJBR and ATJBR decreases with increasing factor activity level. The more severe the factor deficiency, the greater the mean values of ABR, AJBR, ATJBR. (p<0.001).
Table 2.
Mean and median values of HEAD-US, Pettersson, FISH and HJHS scores and annual bleed rate (ABR) in study participants with severe, moderate and mild factor deficiency (n=67)
DISCUSSION
In our study most of the participants presented with joint bleeds, the majority involving the knee (82.46%) followed by the elbow (35.09%) and the ankle (22.81%). In a study among 56 PwH in the Jodhpur region of India, Payal et al. also found the knee to be the predominant joint affected by haemarthrosis (67.85% of cases), but a greater proportion had affected ankle joints (51.7%), followed by the elbow (35.7 %) [22]. The majority of PwH in our study who had affected joints (70.18%) had the knee as a target joint, followed by the elbow (19.30%) and the ankle (10.53%). This is a higher proportion than reported in the observational study of 71 PwH in Western Uttar Pradesh by Mishra et al., who found the knee as the target joint among 57.1% of participants [23]. Of the four PwH with inhibitors in our study, two had both the ankle and the elbow as target joints, and one had the knee, ankle and elbow as target joints. Bleeding episodes are more common in the large complex hinge-like synovial joints of the knee, ankle and elbow, accounting for up to 80% of bleeds in PwH [16,24]. The knee and ankle are subject to more to strain and load than other joints, resulting in microtrauma to the synovium, and the large synovial surfaces of these joints may increase their tendency to bleed [25,26]. Shoulders and hips are better supported and have less weightbearing function, and thus tend to bleed less [25,27].
The amount of tissue factor within the joint also influences bleeding tendency. The knee is the most commonly affected joint in PwH not treated with prophylaxis [20]. We noticed that five patients in our study who had had the knee as their target joint and were on prophylactic factor replacement therapy started experiencing more frequent bleeds in another joint, mainly the ankle. In patients on prophylaxis, the usual pattern of bleeding appears to have changed, with the ankle joint now accounting for the most common site of bleeding.[25]. This may be because current prophylactic regimens, alongside the availability of treatment in the home in many countries, enable PwH to be more active, which could render the ankle the most vulnerable joint.[25]. Twelve of the 18 patients in our study who did not report target joints had mild factor deficiency. Universal Data Collection has shown patients with severe haemophilia to be at a higher risk of developing a target joint than those with moderate and mild haemophilia (33.1% vs. 18.8% and 5%, respectively) [28].
We found a positive correlation between ABR and Pettersson score (r=0.6029, p<0.001), which translates to a 60.29% association between ABR and Pettersson score. Van Dijk et al. found similar results, showing that Pettersson score increased with the cumulative number of joint bleeds, as age progresses [29]. We also found a weak but statistically significant (r=0.2531) positive correlation between age and Pettersson score. As age progresses and bleeding frequency into the joints increases, chronic changes occur to joint anatomy, which can be demonstrated by joint X-ray.
We established a negative correlation (p<0.001) between factor activity level and Pettersson score. Mean Pettersson score was lowest in mild haemophilia group at 1.59±1.66, compared to 11.53±8.01 for severe haemophilia. The more severe the factor deficiency, the higher the annual bleed rate, resulting in more damage to joints, and resulting in a higher Pettersson score. Similar results were reported by Hassan et al. in a study of 50 adolescents with haemophilia A [30], while Fischer et al. found that the Pettersson score increases by 1 point for every three joint haemorrhages occurring after five years of age [31]. People with severe haemophilia have more radiological changes (Pettersson score), as intraarticular bleeding accounts for more than 90% of all serious bleeding events in this population [32].
Our study showed a positive correlation between HJHS and Pettersson scores. (r=0.5774, p<0.001), translating to a 57.74% statistically significant association between HJHS and Pettersson score.
We established a positive correlation between factor activity level and FISH score (p<0.001). The highest mean value FISH score (29.65±2.87) was found in participants with mild haemophilia, and lowest (23.95±4.55) in those with severe haemophilia. Alberto et al. also found the total FISH score to be significantly higher in patients with mild haemophilia (28±0) than in those with moderate (26.27±2.54; p=0.004) or severe haemophilia (24.08±4.74; p=0.0006) in their study [33].
We studied the HJHS 2.1 score as a predictor of HEAD-US and FISH scores using a similar correlation coefficient and regression statistics: HEAD-US score, r=0.6062, p<0.001; FISH score, r=−0.6455, p<0.001. The degree of association with the HJHS score was greatest with HEAD-US, establishing a 60.62% positive association. The study by Guha et al. had similar findings, with a 50% positive correlation between HJHS 2.1 and HEAD-US [13]. We established negative correlation between mean HEAD-US score, mean HJHS score and factor activity level (p<0.001), indicating that the HJHS and HEAD-US score will be higher in severe haemophilia. HEAD-US score versus FISH score had a correlation coefficient (r=−0.6455), giving a 64.55% negative correlation, which is almost the same as Guha et al.'s findings [13]: the greater the functional joint score, the less the joint damage caused by internal bleeding. Altisent et al. assessed joints using HJHS and HEAD-US scores in children with severe haemophilia treated with clotting factor prophylaxis and found them to be concordant in 91/124 (73.4%) joints, inferring that ultrasound using the HEAD-US method can detect a higher percentage of abnormalities than physical evaluation [34].
Our study found highest positive correlation (r=0.6062) between HEAD-US and HJHS score and significant negative correlation(r=−0.6455) between HEAD-US and FISH score. This finding supports the importance of ultrasound as a better tool as compared to X-ray in the assessment and monitoring of target and other joints in PwH and indicates its effectiveness as a tool for the early detection of arthropathy when combined with clinical assessment tools.
LIMITATIONS
This was a hospital-based study involving people who attended our haemophilia clinic during the study period, and therefore may not be wholly representative of the haemophilia population in our region. People with mild haemophilia may not have attended the clinic, and some cases may have been referred to other hospitals where more extensive haematology facilities. Our methodology involved an observational study over one year period; a prospective long-term follow-up study would enable greater understanding the joint health of PwH treated at our haemophilia centre.
CONCLUSION
The drawback of using only clinical and functional assessment of joints in PwH is that we may miss the early changes which can be picked by radiological assessment. MRI remains the gold standard procedure for radiological assessment of joints, but its use is not feasible in a low-resource setting. Our study found ultrasound scoring (HEAD-US) to be a better diagnostic tool in comparison to X-ray (Pettersson) when used in combination with clinical assessment. Combining tools like HJHS, FISH and HEAD-US can provide a cheap, quick, more reliable and accurate option for the consistent assessment of haemophilic joints and may help support the optimisation of management of joint damage in resource-constrained settings like India.