Haemophilia A and B are X-chromosomal recessive coagulation disorders occurring at an incidence of 1/5,000 and 1/25,000 births, respectively [1,2]. Depending on the severity of the disease, patients with haemophilia may develop extensive bleeding following injury or surgery but also spontaneously. Unrecognised or untreated bleeding episodes may cause severe morbidity such as haemophilic arthropathy. In the last decades, several studies have clearly demonstrated that early prophylactic factor replacement significantly reduces bleeding events and the risk of joint damage in patients with severe haemophilia [3,4,5].
During their teen years, adolescents are faced with several changes in their physical, cognitive, and psychosocial development. The most important tasks of this transition period include the development of advanced reasoning skills, identity, and independence from parents [6]. Accomplishment of these tasks involves experimenting with different ways of appearing, sounding and behaving; risk taking; and managing orientation towards peers and being accepted by them [6, 7, 8, 9]. Carrying a chronic disease in this phase of life may lead affected teens to believe that they are different from their peers. The intense desire to belong to a particular group can influence teens with chronic disease to undertake dangerous activities that may negatively affect the course of the disease [10]. Therapies for a chronic condition may strongly interfere with the struggle for autonomy and the pressure for conformity.
Adherence is a challenge when caring for adolescents with haemophilia [14,7,8,10]. Poor understanding of the disease, individual perception of treatment efficacy, bleeding pattern, costs, and the relationship with the care team can have an impact on adherence in this age group [4,8,9,11,12, 13]. By contrast, adherence may be facilitated through cooperative decision making about treatment, support from family, and making the handling of factor products as simple as possible [4,11,12,14]. Adherence is a generic term for acceptance, persistence and compliance [15,16]. “Non-acceptance” means not having a medical prescription filled, “non-persistence” is when the patient autonomously terminates treatment, and “non-compliance” means unreliable medicine intake. The most important prerequisite for adherence is shared decision making [17,18]. Adolescents must receive targeted and comprehensive information on both the disease and the benefits of treatment, and develop the ability to act as a partner in shared decision-making [19]. The process of transferring responsibility to adolescents should be such that it enables them to be adherent and to develop autonomous and responsible health related behaviours [20, 21, 22, 23, 24, 25]. The study by Khair and colleagues (2013) recommends for the United Kingdom tailored interventions for children and early adolescents dealing with illness and therapy, rather than formalised training programmes [19]. In reviewing the literature no data was found about how to guide haemophiliacs in Switzerland towards autonomous and responsible self-management and adherence. A prerequisite in the search for such answers is an understanding of the adolescent mind-set. This study therefore aimed to investigate the process of adherence to treatment in adolescents with haemophilia in Switzerland by exploring the inside views of the adolescents themselves.
Materials and methods
A qualitative design, the Grounded Theory methodology, was chosen following Charmaz’ constructivist approach, explained elsewhere [26,27]. Ethical approval was given by the Ethics Committee of the Canton of Zurich, Switzerland (KEK-ZH-Nr. 2011-0443).
Patient population
The study population includes adolescents with haemophilia A or B, aged 15-25 years. All patients are followed at the University Hospital and University Children’s Hospital of Zürich, which constitutes the largest Haemophilia Reference Centre of Switzerland. Only patients able to read and speak German were asked to participate in the study. All patients and, for those 15 to 17 years old, their parents, gave written informed consent.
Data collection and analysis
Contact information was available for 22 potential subjects. The initial sample was extended by theoretical sampling during the data collection procedure [26]. In total, 16 adolescents were asked to participate. Three adolescents refused. One of them due to a stay abroad, two of them were in the midst of school exams. After 13 interviews no new categories emerged, indicating data saturation.
Single interviews (n=13) were conducted between April and June 2012 using theoretical sampling (Table 1). Demographic data and information about the type, severity and treatment regimen of haemophilia were obtained by questionnaire. The sample comprised all three degrees of haemophilia severity.
The participants, frequencies and averages of sociodemographic factors were computed with PASW Statistics 18. The interviews were transcribed verbatim and analysed according to the Grounded Theory method, using ATLAS.ti 6.2 software. The analytical process and data collection were subject to constant comparison [26]. Peer group discussions and member checking were performed.
Patient population
The participants were all male with an average age of 17.5 years, as shown in Table 2. Eleven participants had haemophilia A, two had haemophilia B. Six had severe, three moderate and four had mild haemophilia. Five received prophylactic treatment. All participants managed their treatment themselves, as summarised in Table 3. After 13 interviews no new categories emerged, indicating data saturation.
Table 2
Demographic characteristics of adolescents (n=13)
Table 3
Participants interview ID and characteristics
| ID | Age (years) | Type and severity | Treatment regimen | Who does the treatment* |
|---|---|---|---|---|
| 1 | 22 | A severe | P 3x/week | Boy |
| 2 | 16 | B moderate | P 2x/week | Boy, mother, father |
| 3 | 18 | A mild | OD | Boy |
| 4 | 16 | A severe | P 2x/week | Boy |
| 5 | 16 | A severe | P 2x/week | Boy |
| 6 | 18 | A severe | OD | Boy, mother |
| 7 | 20 | A severe | OD | Boy |
| 8 | 17 | A moderate | OD | Boy |
| 9 | 19 | A moderate | OD | Boy (mother) |
| 10 | 15 | A mild | OD | Boy, mother |
| 11 | 15 | B severe | P 2x/week | Boy |
| 12 | 18 | A mild | OD | Boy (mother) |
| 13 | 18 | A mild | OD | Boy (mother) |
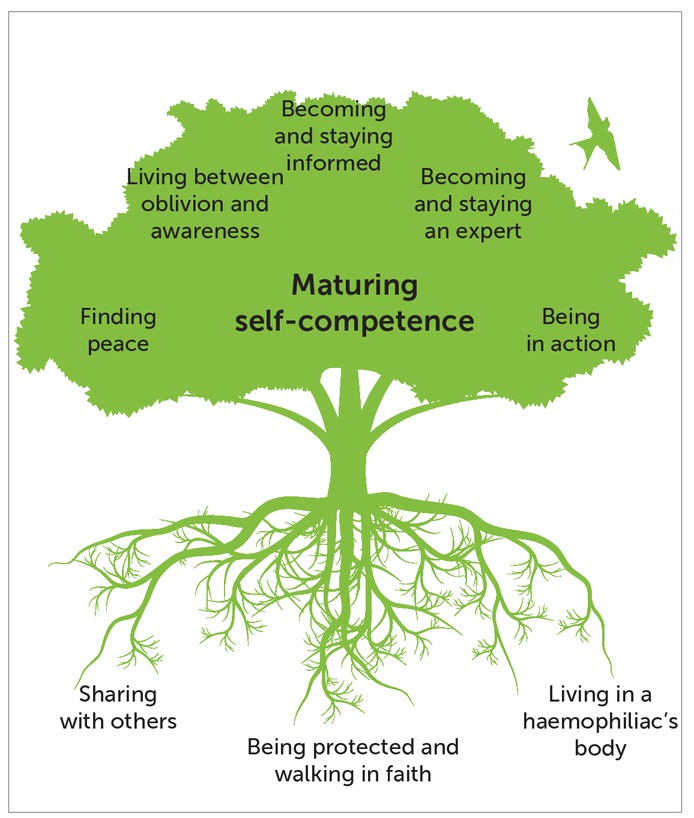
Maturing self-competence
The core category "maturing self-competence" describes a continuous development process throughout childhood towards a confident decision for their own therapy regimen. "Maturing self-competence" generally manifests itself as a passive social process that enables adolescents to undertake self-management. In this process, their experience emerges as a central element. Everyday decisions for or against adherent behaviour are guided by the state of "maturing self-competence". Generally, adolescents see themselves as having grown into their haemophilia experience and thus as being self-competent.
“I already have 16 years of experience now. I can really judge how it’s going." ID 5
In the model developed, the multiple layers of factors affecting adherence in adolescents with haemophilia are shown in Figure 1. The three constitutive categories "living in a haemophiliac’s body", "sharing with others" and "being protected and walking in faith" represent basic experiences in the adolescent’s life. Five emergent categories arise from these basic experiences:
Becoming and staying informed
Becoming and staying an expert
Being in action
Living between oblivion and awareness
Finding peace.
In all categories, a continuous development process was observed. All categories stand in a mutually influencing relationship and guide adolescents in the decision-making process regarding adherence.
Living in a haemophiliac’s body
The category "living in a haemophiliac’s body" represents statements reflecting the adolescent’s physical awareness. Adolescents had extreme experiences that strongly impressed the presence and the consequences of haemophilia on them.
"Yes, it’s simply, like, like having come from one day to the other. I just noticed it won’t work anymore ... Bleeding, yes, elbow, foot, just everywhere. And even though I always treated myself." ID 2
Self-treatment is a constantly recurrent challenge. Interviews show that the relationship of the adolescents to self-harming therapy is ambivalent: on the one hand, injections are part of normal life; on the other hand, they are onerous and tedious.
"Yes, from time to time it pisses me off, treating myself ... Or, I think, that’s just part of it, that’s with all you have to do, it’s just that you don’t feel like it, and so ..." ID 12
Sharing with others
The category "sharing with others" represents statements regarding interactions in the social context. Therein, adolescents oscillate between the poles of "being different” and “not being different". This was evident with all participants. Having to perform therapeutic procedures gives haemophiliacs the feeling of "being different".
"It literally pisses me off having to draw up the syringe and to treat myself and clean up everything. Just the entire procedure, it gets on my nerves. That’s also the only moment when I feel I’m a bleeder, except when I have a really hard bleed … not because "oh man, I’m a bleeder" but rather because of "oh no, I have to treat myself" … That’s simply the moment when you notice, now you have to spend time in something the others never have to." ID 4
Likewise, the care or special attention from others can be experienced as "being different".
"Yes, but afterwards I did not do it [informing others] any longer, because afterwards these things happened, that I did not want to happen ... Just the compassion and all that. And after that I really was the special case." ID 3
Adolescents experienced a polarity of both respectful and emphatic reactions in the social setting and not being respected and understood. When considering informing others, an appraisal of whether the social context would be respectful and empathetic was defined. Nevertheless, adolescents deem it useful to inform those in their environment. They count on receiving support in case of an accident or bleeding event.
"Well, I don't know, it kind of depends on the situation.
When there's a class where the relations are not so good, when there could be stupid jokes all the time, yes. Well, no (hesitates) I would do it. It's just good if they know. If something happens, then it's really better." ID 1
Being protected and walking in faith
The category "being protected and walking in faith" is derived from statements about experiences with guardian angels. Adolescents went through critical events without negative consequences. Haemophiliacs also compared themselves to others, for example with regard to number of substitutions, frequency of bleeds and their range of motion.
"I'm quite a lucky fellow (laughs), being a bleeder. Well, I don't have as many bleeds as others. And that's why I don't feel strongly limited." ID 5
Becoming and staying informed
The category "becoming and staying informed" comprises the process of collecting information on self-management. Knowledge is passively accumulated and assimilated when children are present during discussions between physicians and parents. Readiness for knowledge transfer does not develop at a particular age. Over the years, adolescents consider themselves independently informed about whether information is correct or not.
"But the theory and such, I learnt that in parallel, over the years. I was able to treat myself. I injected the medication, it’s good for me, and I did not want to know more and I didn’t need it. It does not have any side effects and so on, and that’s why I found I don’t have to check anything." ID 4
Adolescents wished for a proactive information strategy: they wished for more constructive information rather than being told what is prohibited.
"Just more, as I just said, just give more alternatives about what you can do as a bleeder." ID 4
Becoming and staying an expert
The category "becoming and staying an expert" represents the adolescent experience with regard to decision-making. Daily life experiences with the disease become the basis for self-made decision concepts in dealing with haemophilia. This gradual development of individual expertise must be taken into consideration when dealing with adolescents.
"And mainly the older you get with this disease, the more experience you have. Then you know, yes it helps me, or whether you might as well forget that. You have to look at things individually. It’s not that you can say every bleeder is so and so." ID 9
Adolescents are convinced that having haemophilia helps them better understand themselves.
"I also think by that being a haemophilic, I also have a better understanding of my own body … It's just a physical feeling and it just evolves over the years." ID 12
Some adolescents on prophylaxis are convinced that prophylactic treatment is important to prevent bleeding. "Prophylaxis. Regularly. Yes (pauses). And, like, looking after oneself." ID 2
Others say that occasional self-treatment is sufficient. "I just see to it that I have my injections from time to time." ID 9
Being in action
The category "being in action" describes adolescents taking active and deliberate decisions to cope with and plan for different aspects of everyday life. As they take responsibility for the therapy, prophylaxis is tailored to their daily rhythm. This necessitates the capacity for self-treatment. While prophylaxis should preferably be performed in the morning, the majority of adolescents consider the morning hours unfavourable.
"I don’t know, it bugs me to treat myself early in the morning, but otherwise, it doesn’t really … At the moment I am able to arrange to come home over lunch and to treat myself. So still before sports." ID 10
The symptoms strategies of adolescents show a balancing between symptoms of an acute bleed and the regular treatment regimen.
"Sometimes I don’t feel like it, and when there’s nothing, then you think you might as well leave it … Yes, ha, but that’s only when there is nothing. Otherwise I really do it consistently." ID 1
The therapy can be perceived as a nuisance, be simply forgotten, or patients may not like injections. "Yes, firstly I always forget it. Secondly, I don’t feel like it or I’m too tired when I think of it. Or in the evening, when I’m falling asleep, then I think of it. Well, but I could have." ID 9
The presence of bleeding symptoms indicates whether or not treatment is necessary.
"When I feel something in a joint, then I'll treat myself right away. I can slowly feel that it is bleed. It's like a reaction." ID 5
Living between oblivion and awareness
The category "living between oblivion and awareness" describes the ambivalent behaviour of adolescents between being conscious of and forgetting about haemophilia in daily life. Basically, adolescents live as if they had no haemophilia.
"Actually, I don’t think about it. Except when something hurts, then I think, alright, it’s time to treat myself again. Then I think of the disease, but otherwise, in daily life, hardly ever." ID 9
Finding peace
The category "finding peace" describes the attitude of adolescents towards haemophilia and how they accept it as part of themselves. Adolescents compare haemophilia with other diseases.
"In the end you have to say, better a bleeder than some other things." ID 4
Acceptance is accompanied by different emotions. Even patients who have completely accepted the disease may experience moments of rebellion.
"Well now I have this, I accept it and that’s the way it is. Of course there were moments when it completely pissed me off, when I, totally, ehm, was depressed, well, yes. Maybe two days or so, because I had something, or so. And why me? And why can’t I be, and so? But then I also thought it’s something that you can live with. It does not really burden me a lot in daily life, or actually not at all. And if it does, then it’s so that I know and that I can watch it and keep it under control." ID 9
Carrying a congenital disease is seen by some as a help in learning how to deal with haemophilia through life long experience.
"In a way I was lucky to have been born with this, maybe this sounds stupid, because I grew up with this, I gained experience, I shall go on gaining experience, and one day I’ll die with it." ID 13
Discussion
Medical care of adolescents with haemophilia is often complicated by poor adherence to treatment. The developed model "maturing self-competence" represents the complexity of factors influencing adherence. Adolescents essentially perceive the therapy as a nuisance, therefore they try to get along with as few substitutions as possible. The experience of getting through critical situations without being affected can lead adolescents to a misleading impression of being protected and untouchable. They describe their expert knowledge as resulting from an evolving process. Reflection upon experiment-based experience grows into an individualised concept of how to approach the therapy. Decisions concerning adherence depend on the stage in the "maturing self-competence" process and on the adolescent’s situation-dependent assessment. As they grow they perceive themselves to be self-competent.
An understanding of disease and illness beliefs, perceptions of the efficacy and benefits of medicine, influences compliance [4,8,9,11,13,28,]. The present study provides insights in their evolution. They are developed through personal experience with haemophilia. This process is accompanied by passive knowledge accumulation from childhood through adolescence. This study shows that there is no moment in adolescence that is particularly suited for improving disease understanding. Interest in information on the disease is low. This implies that knowledge about haemophilia ought to be imparted before the onset of puberty.
Rare bleeding events influence adherence [4,12,14]. Results of the present study support and extend the assumption that adolescents feel entitled to forget about haemophilia in their daily life when there is infrequent bleeding, and to consider ongoing treatment regimens unnecessary [4,12]. Adolescents live with the simultaneity of oblivion and the presence of haemophilia.
A trustful partnership between adolescent patients and medical staff plays a major role in adherence for suggested treatment modalities [17,28]. The study underlines the necessity for adolescents to be considered self-competent partners in defining and adapting the treatment regimen according to the clinical situation and their current lifestyle. Only the basic attitude of shared decision-making makes adherence possible. The factors mentioned in the literature, i.e. treatment cost, handling and safety of the products did not present themselves as influencing adherence in the present study [11,12,4].
The results of this study show that adherence is influenced by the adolescent’s inner decision concepts and by the strong urge not to be different from their peers [6]. The definition of adherence described by Füessl and Middeke (2010) is confirmed and extended, accounting for the lifestyle of adolescents [15]. A new precondition for acceptance turned out to be acceptance of the disease and its causes. Persistence is implemented through situational adaptation of the treatment regime to daily life. Compliance, defined as obedience to medical staff, does not have a place in adolescence. Adolescents want to be respected as self-competent and be partners in defining their therapy. Only a basic attitude of shared decision-making makes adherence possible [16,17,29].
Quality criteria for this study are credibility, originality, resonance and usefulness, verified by discussions among the authors [26]. Peer debriefing with the first and the last author further supported transferability, dependability and confirmability, ensuring trustworthiness [30,31]. Furthermore, the sample comprises all three degrees of haemophilia severity. Data saturation is assumed since the analysis of the interviews did not show any new categories. The study is limited in that participants were recruited from a single centre only. The complexity of the decision-making process regarding adherent behaviour is expressed by the model "maturing self-competence". The model should be verified for different severities of haemophilia.
Conclusion
As they grow from childhood to adolescence, a haemophiliac’s perception of the disease grows with them, fed by knowledge gleaned randomly from their presence at medical consultations and from experience with their own body’s reaction in daily life and under extreme occurrences. The stage in this "maturing self-competence" and the adolescents’ assessment of the situation at hand form the basis for decisions concerning adherence.