Haemophilia is generally considered to be a male disease and is viewed mainly in the context of severe deficiency. Blackwell’s Dictionary of Nursing [1] defines haemophilia as “an inherited bleeding disease found only in males and transmitted through carrier females, who are daughters of affected males.” It also states that in “special genetic circumstances, females with haemophilia may be produced” and that sufferers are subjected “to prolonged bleeding following minor injuries.” This definition is not entirely accurate, as carriers are not solely the daughters of men with haemophilia but may be the daughter of a carrier or a long line of carriers. The Merriam-Webster Dictionary [2] defines haemophilia as a “sex-linked hereditary blood defect that occurs almost exclusively in males and is characterized by delayed clotting of the blood and consequent difficulty in controlling hemorrhage even after minor injuries.”
The emphasis remains on a severe, male condition. In The Bleeding Disease: Hemophilia and the Unintended Consequences of Medical Progress, Pemberton, a medical historian who worked with Dr Kenneth Brinkhous, one of the leading pathologists of the last century, writes about the historical context of haemophilia and the anomalies of its definition [3]. He chronicles what he sees as a “story of gender and social identities repeatedly negotiated, challenged and redefined,” [3]. Although the earliest known record of haemophilia was found in writings of Jewish law dating to the 2nd century it wasn’t until the beginning of the 19th century that physicians began to try to understand the hereditary nature of haemophilia [3]. There was acknowledgement of bleeding among females, yet by the first decade of the 20th century the definition that defined haemophilia was “an inherited tendency in males to bleed” [4]. The means of diagnosis at the time relied solely on the physical manifestations of moderate to severe disease such as joint and muscle bleeds and the fact that the affected individual was male. Haemophilia was viewed as having no physical affect on women; carriers became viewed as just that, a carrier. In the context of American and European societies in the first half of the last century, where women were not viewed as equal to men and there was a the lack of expertise available to make more clear diagnoses, women’s symptoms and risks of haemophilia were largely ignored. As medicine progressed and the complexities of bleeding disorders became better understood the notion that women could be affected began to be recognised. Even so, Pemberton [3] argues the “masculine concept of haemophilia” was advanced by haematologists of the 1950s as it “highlighted the severest type of hereditary bleeding” [3]. This concept, he argues, was also vigorously supported and promoted by the National Hemophilia Foundation (NHF) in the United States, along with other national haemophilia associations. To this day the language used in most professional literature continues to designate the diagnosis of haemophilia to men only, while separating women into a diagnosis of affected or unaffected carriers.
Table 1
Number of females registered on UK National Haemophilia Database in 2013 (figures from annual report available from UKHCDO)
In 2000, the International Society on Thrombosis and Haemostasis (ISTH) published guidelines on the Classification of severity of haemophilia in a bid to standardise the three different levels of haemophilia A and B worldwide [5]. It adopted a classification based solely on the individual’s plasma levels, with <0.01IU/ml being severe, 0.01-0.05IU/ml being moderate and >0.05-<0.40IU/ml being mild. Although it is recognised that there are varying bleeding phenotypes among individuals with haemophilia, the ISTH recommendation was that for the purposes of definition only plasma levels be used. There is no gender distinction allocated to these levels.
In its monograph entitled Symptomatic Carriers of Hemophilia, the World Federation of Hemophilia (WFH) acknowledges that carriers have bleeding symptoms and clotting factors in the same range as men but falls short of allocating affected women the diagnosis of haemophilia [6]. If using the ISTH classification there can be no distinction between the sexes as the severities of factor VIII and factor IX deficiencies are based solely on plasma levels of the circulating factor not phenotype or gender.
WFH accepts that women may have mild haemophilia
The most recent WFH management guideline poses the question “What is haemophilia?” giving an 8-point outline beginning with the statement that it is “an X-linked congenital bleeding disorder caused by a deficiency of coagulation factor” and that it “generally affects males on the maternal side”, ending with the statement that “A definitive diagnosis depends on factor assay to demonstrate deficiency of FVIII or FIX” [7]. Although most of the text does not specify the affected individual as male or female, section two, under “Special management issues” specifically addresses women with haemophilia under the subheading of “Carriers.” Here WFH acknowledges that some carriers have factor levels in the “haemophilia range”, generally in the mild range except for rare cases of extreme lyonization. The guideline acknowledges that “carriers with low clotting factor levels should be categorised as having hemophilia of appropriate severity and managed accordingly”. Despite this, throughout the world most women are not categorised as such and remain unaware of their status, unmonitored and potentially at greater risk than their male counterparts, who are likely to have a diagnosis of haemophilia. This is particularly important in light of the gynaecological risks that women face. Perhaps, this is largely due to most women having mild haemophilia, which has traditionally received less attention, even for men. Inhibitor risk, however, is one area that affects men with mild haemophilia and not women. [8] Even so, women should be given the same care and attention afforded to men with mild haemophilia.
The United Kingdom Haemophilia Centre Doctors’ Organisation (UKHCDO) devotes only one paragraph to affected women in its Practice Guidelines for the Molecular Diagnosis of Haemophilia A and B [9]. Although the severity categories follow the ISTH guidelines, the UKHCDO states that carrier females with levels of below 30% are at risk of bleeding. Why a different threshold for women? Other than these brief mentions, women are really only discussed in the context of carrier status. Perhaps it is no wonder that the diagnosis of haemophilia is rarely imparted to women.
Historically haemophilia has been seen as a male condition and this view is reflected in the population-based incidence data collected in different countries. In a 1998 paper on the occurrence of haemophilia in the US, the criteria used by the Centers for Disease Control and Prevention (CDC) was that of a “person with physician-diagnosed hemophilia A or B and a baseline clotting factor activity level of < 30%” but carriers of haemophilia were blatantly excluded [10]. Although the authors reported the need for studies to justify medical resources, identify those at risk of complications, to plan and prioritise local preventative healthcare strategies and disseminate accurate information to the community, a large proportion of affected individuals were omitted based on gender. This lack of included women was not because they were in the mild category: the authors deliberately conducted their survey over three years in an attempt to ensure the inclusion of those with mild haemophilia. They noted for mild haemophilia the need to be seen at a haemophilia treatment centre was less than those with severe or moderate haemophilia.
In 2009 the CDC, acknowledged that its method of data collection did not target female-related bleeding symptoms and did not represent the burden among females. It then began collecting data separately, focusing on women with bleeding disorders [11], principally women with von Willebrand’s disease, the most common bleeding disorder. CDC conceded that at the time of publication the sample size was still too small but concluded that females with bleeding disorders required national and international attention and resources in order to improve care for women worldwide.
In its monograph on Mild Hemophilia [12] WFH highlighted the contradictions that continue to exist. It acknowledges that different publications vary significantly by including or excluding people depending on the normal ranges used. Changes in attitudes and definitions are beginning to occur: the recent WFH publication Carriers and Women with Hemophilia puts women with corresponding clotting factor levels on a par with men [13].
Data quality issues
Stonebraker et al [14,15] reporting the differences of haemophilia A and B throughout the world, highlight the difficulties in assessing the true numbers of men affected by the condition let alone women whose diagnosis is usually secondary to a family history of the disease or an affected child. They also question the quality of data; it is unclear whether differing healthcare systems report the same quality of data.
Countries that offer universal access to healthcare, such as the UK, are more likely to identify people with haemophilia even if they do not require treatment. Surveillance and registration of haemophilia carriers in the UK could be seen as relatively good in comparison to many countries, although the consistency and thoroughness of reporting may vary between centres. This variation is likely given that centres often have different attitudes to treatment, and staffing levels may hinder follow up of extended family members from each affected individual. While most acknowledge a distinction between affected and non-affected carriers, the diagnosis of haemophilia is rarely used. The UK National Haemophilia Database does not categorise women as having haemophilia but rather gives the option to register them as haemophilia carriers or females with VIII or IX deficiency [9]. The impact of this is lessened by free access to treatment and therefore the significance from a treatment point of view is less than in the US, where diagnosis is important to obtain healthcare coverage.
In countries with less developed healthcare systems and poor economic status, it is even less likely that women with haemophilia would gain access to treatment. Stonebraker et al [14] analysed the global use of factor IX treatment and found a positive correlation with economic capacity. They acknowledged that data could be skewed by the under reporting of haemophilia B with evidence suggesting that most would be unlikely to report women in these figures [14,15].
Just how many females with haemophilia there are globally is difficult to estimate as little data exists. It is evident that a large proportion of women are not identified. In trying to estimate haemophilia carrier numbers in relation to affected men, Kasper and Lin [16] reviewed 731 pedigrees of families with haemophilia and found that for every 100 men with haemophilia there were over 150 somatic carriers. A significant number of these women would have had factor levels that fall in the mild haemophilia range, yet until recently most would never have been tested. Winikoff et al suggest that 10% of haemophilia carriers are ‘affected’ with levels in the haemophilia range [17] while others cite a figure as high as 30% [18]. The WFH puts a global estimate for women with haemophilia at almost equivalent to men with haemophilia A [19].
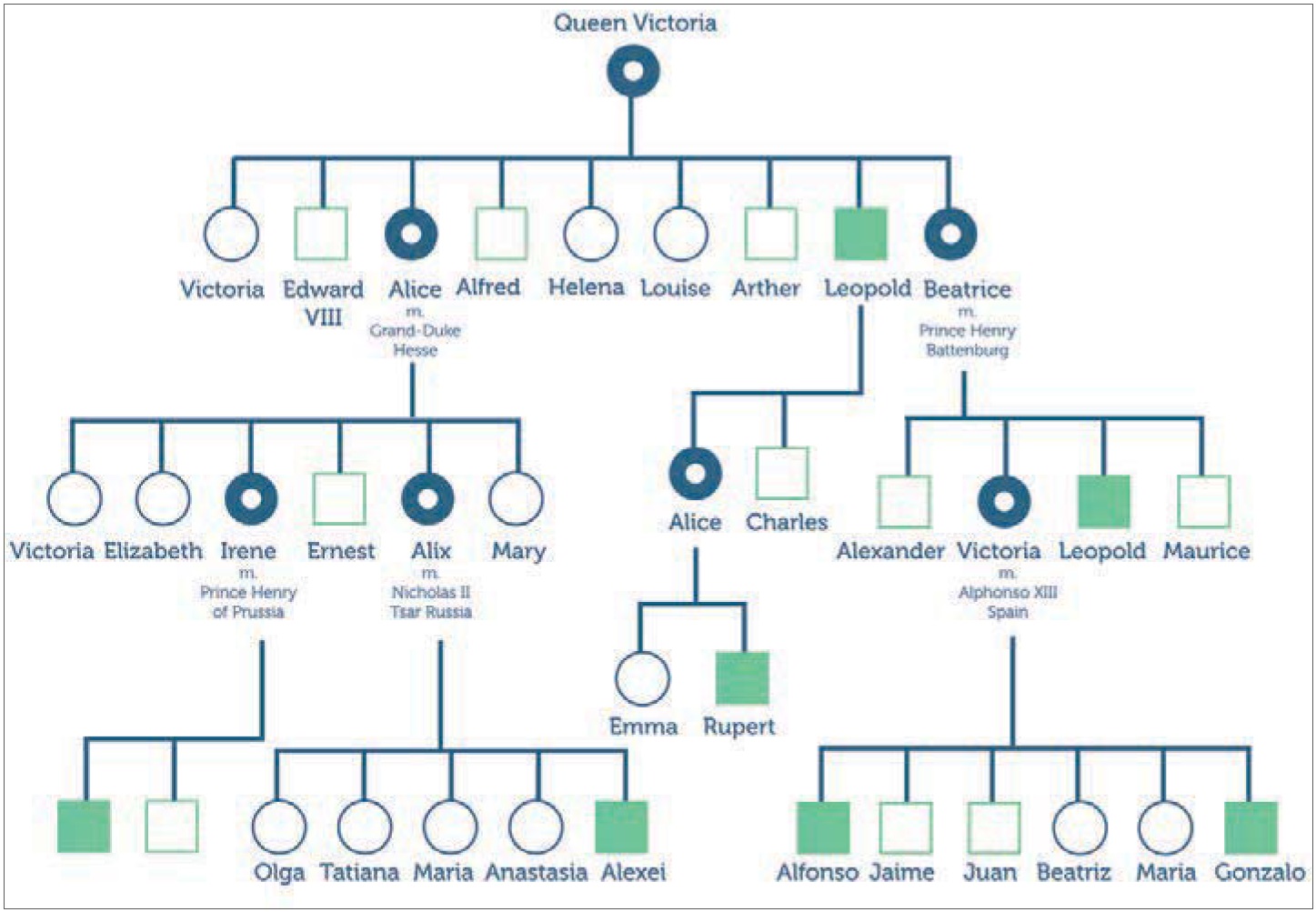
The difficulty in identifying carriers is illustrated by Queen Victoria: had she only had two children her carrier status would have been unknown [16]. As recently as the 1980s haemophilia carriers were diagnosed using pedigree analysis and/or factor levels [20] rather than genetic testing. It is likely that there are a significant number of women who were given incorrect diagnosis from this and therefore subsequent generations may have gone undiagnosed.
Emotional and behavioural issues in carriers
Renault et al [21] studied the emotional and behavioural responses of haemophilia A carriers, highlighting many of the issues that are perpetuated by narrow thinking and historical definitions and how these have had a negative effect on women’s lives. Negative feelings were generated by misinformation about haemophilia in women, both among healthcare providers and the general public. It is ironic that this study still refers almost solely to affected women as carriers, further demonstrating that women with mild haemophilia are perceived differently than men with mild haemophilia. One interesting point they make is that part of the problem for many of the women is that “gynaecological and obstetrical bleeding are unique to affected females, and are thus not characteristic symptoms of a disease classically associated with males.”
Although women with haemophilia have the same bleeding risk following haemostatic challenges as men, the issue that sets them apart is the gynaecological and obstetrical bleeding problems that dominate their lives and can affect quality of life [21, 22]. Menorrhagia is the most frequent and common problem experienced by women with bleeding disorders but there are many other manifestations that put women at risk including haemorrhagic ovarian cysts, endometriosis, anovulation, polyps, fibroids, pregnancy and miscarriage [23].
It is widely recognised that clotting factor levels rise in pregnancy but they do not always do so, particularly with haemophilia B, thus these women are more at risk of bleeding and need to be managed accordingly [24, 25]. Therefore ‘carrier’ status needs to be recognised including their diagnosis of haemophilia as this could affect the treatment they receive, particularly outside the safety of a haemophilia treatment centre. It is likely that the preconceptions of a woman being ‘just’ a carrier passing on the affected genes will be seen here.
The age issue
It is not only obstetric and gynaecological issues that are important in the management of women with haemophilia but also issues that arise with age and the increasing need for surgical interventions, particularly as a result of trauma and emergency situations. The impact of mild haemophilia on an ageing population of men with haemophilia has recently become an area of focus for health professionals. As medical knowledge advances and more treatments and procedures become available, understanding outcomes and impacts for this cohort, whether male or female, is becoming necessary. Older men with haemophilia are at the forefront of investigation and research, and are demonstrating the limitations of the knowledge base around mild disease. Franchini et al [26] and Peerlink and Jacquemin [27] acknowledge the challenges of managing ageing men with mild haemophilia.
Like men, women are at risk of heart disease, need increasing surgical interventions and therefore, a require better understanding of how to balance their complex needs given that to date they have largely been excluded from research and evidence based care. In the context of trauma or emergency situations a clear diagnosis could save a life.
Literature investigating the psychosocial impact of haemophilia in women focuses on carrier status and the impact, or potential impact, of having a child with haemophilia. It stresses the idea of ‘carrier guilt’ and the impact of this on reproductive choices [28], largely attributable to women, fuelled by the historical view that men are affected and women are the route for its continued transmission through the generations. In the meta-analysis of the psychosocial impact of haemophilia by Cassis et al [28], there were no studies reporting the impact of men with haemophilia passing on the affected gene but several investigating the impact and reproductive choices for women. Yet, as we know, daughters of men with haemophilia are obligate carriers and many also have haemophilia, so why the concept of guilt is always attributed to the female members of families remains to be answered. If such ‘guilt’ exists it should be equally attributed to or examined in men with haemophilia.
The importance of a diagnosis
In Putting a Name to It: Diagnosis in Contemporary Society, Jutel [29] examines the importance of medical diagnoses. These, she argues, have the ability to “confirm status and allocate resources”, therefore becoming the basis for groups of affected people jostling for funding and recognition [29]. In the context of haemophilia this focus has helped haemophilia groups, particularly in western societies to gain recognition and, following the AIDS disaster, a strong political influence.
Jutel states that diagnoses develop out of social contexts and can become a source of collective identity removing the sense of isolation, promoting a potential network of support [29]. In the UK and US the network of support for women with bleeding disorders has continued to grow through the UK Haemophilia Society’s Women Bleed Too [30] website and the NHF’s web site Victory for Women initiative [31]. The Française des Hémophiles in France acknowledges that women have haemophilia and has established a women’s commission to support and be a voice for women [32]. For women to benefit from these support groups they need to be identified, and organisations and groups publicised in an accessible manner. The Internet makes this possible but it remains the role of the haemophilia treatment centre to ensure the availability of accurate information and support.
The WFH has accepted the need to acknowledge and include women with haemophilia and other bleeding disorders [19]. The need for continued efforts “to enhance diagnosis and access to treatment for under-recognized populations particularly women” was cited as part of the next phase of the Global Alliance for Progress. In a move to acknowledge this, the WFH website states that “Any person (male or female) with 5-40% of the normal amount of clotting factor has mild hemophilia” [33]. This statement confers the importance of equal diagnosis giving women a sense of inclusion in a collective diagnosis.
The NHF has been increasing support for the need for an inclusive diagnosis to be made. Koerper [34] argues that by the medical definition of ’carrier’ the concept of a ‘symptomatic carrier’ is not a valid diagnosis. The significance of this is particularly apparent where insurance companies will only fund clotting factor treatments for a clear diagnosis of haemophilia. In The Carrier Barrier, Aldridge explores the difficulties arising from an inadequate diagnosis from a patient perspective, recounting examples that continue to confront women, whose diagnosis of a ‘symptomatic carrier’ is wholly inadequate and illustrates the boundaries between them and men [35].
By being denied a diagnosis of haemophilia, many women during the 1970s and 80s escaped the tragedy of blood-borne viruses when more than half of the US haemophilia population was infected by HIV [36]. Contaminated factor products may well have been used by women diagnosed with haemophilia more readily than they were, therefore exposing them to hepatitis B, C and HIV. How this impacted upon men with mild haemophilia can be seen by the significantly lower number of Italian men with mild haemophilia who contracted HIV as DDAVP was used earlier than in the US, where DDAVP was not licensed until 1984 [37]. The prevalence of HIV infection among this cohort was nine times more than in Italy [37].
Although the threat of blood-borne viruses has been theoretically eliminated by the development and use of recombinant products, it remains in countries where access to products is limited, even for those with severe haemophilia. For women with haemophilia in developed countries the advantages of haemophilia being recognised equally to men brings greater understanding of its’ impact upon women and their lives
Conclusion
Examination of the haemophilia literature does not appear to offer any solid reason why “affected” women have not been afforded the diagnosis of haemophilia, other than through the historical context of how haemophilia has been perceived. Although these perceptions are beginning to change, there is evidence that haemophilia is still a long way from being accepted as a clear diagnosis in females.
Haemophilia is a rare disorder. It is well recognised that men with severe haemophilia, the most recognised and well-defined cohort, suffer from misunderstandings and mistreatment. In order for women to obtain a consistent diagnosis of haemophilia and be treated as such, the specialists who work in this area need to change the language they use to dispel old perceptions. Only then will affected women have an opportunity to have their condition validated and be seen equally to their male counterparts.
If the WFH estimates are correct, a huge number of women worldwide receive suboptimal care and have to live with the psychosocial consequences. The care of these women worldwide can be improved. As argued here, the girls and women in families with haemophilia are not just carriers; they are people with haemophilia too and should be recognised as such.
Queen Victoria had four sons (squares) and five daughters (circles). One son had haemophilia B (solid square) and two daughters were known to carry the gene (dotted circle), passing it on to boys in the Spanish and Russian royal families. If she had only had two children, Victoria’s carrier status would have remained unknown