The life expectancy of a person with haemophilia (PWH) was only 20 years in 1960, but is now almost the same as the national average [1]. Part of this improvement is due to diagnostic and treatment advances, as well as the expertise of those providing care to this population. Since 1966 it has been recognised that the management of haemophilia and other bleeding disorders requires expertise and input from a variety of disciplines [2, 3, 4, 5].
Early studies verified that care based at a haemophilia treatment centre (HTC) drastically improved many haemophilia-related physical and economic outcomes [5, 6]. The core HTC team historically consisted of a physician, social worker, physical therapist and nurse. Over time, the core team has expanded to include advanced practice providers (APPs), specifically nurse practitioners (NPs) and physician assistants (PAs). This evolution has been partly fuelled by the shortage of trained haematologists [8, 9, 10, 11]. Consistent with the Institute of Medicine’s (IOM) concept of team-based care, the HTC team focuses on collaboration to provide coordinated, high quality and patient-centred care [7]. As the intricacies of caring for those with bleeding disorders increases, it has become more difficult to find haematologists who are interested in subspecialising in bleeding disorders, leading to medical staffing issues at many HTCs across the United States [8, 9, 10, 11]. Where there is a gap, APPs have filled that role [12,13]. Both NPs and nurses have a larger role in the business management and funding of HTCs, with funding coming through multiple sources including federal and state grants, direct billing for services rendered and, in some cases, program income generated through 340B pharmacy programs [14].
The Nursing Role and Responsibilities
In the United States, registered nurses typically have an associates or bachelor’s degree in nursing. NPs are advanced practice registered nurses (APRNs) with a master’s degree or doctorate in nursing, with advanced clinical training and expertise in diagnosing and treating health conditions, including pharmacology to prescribe medications, that prepare them to practice in multiple settings. NPs are licensed in all states and the District of Columbia, practicing autonomously and in collaboration with other healthcare professionals under the rules and regulations of the state in which they are licensed [15]. Physician assistants (PAs) complete a postgraduate program based on the medical model, usually leading to a master’s degree, which also focuses on clinical training and expertise in diagnosing and treating health conditions, including prescribing medications [16].
US HTC nurses provide their expertise in direct patient care, education, advocacy, research and coordination of the entire HTC program. They also teach home infusion, thus increasing independence and reducing delays in bleed management. The HTC nurse is often the primary point of contact for patients and families; evaluation and treatment is expedited when calls are triaged by an experienced haemophilia nurse [17]. While expert haemophilia nurses play an invaluable role in improving outcomes, little has been written about how they formally develop this expertise, the differentiation between the nursing roles and the APP role, and how their ongoing education is supported. In 2015, the European Association of Haemophilia and Allied Disorders (EAHAD) Nurses’ Committee developed a curriculum to standardise and benchmark haemophilia nursing care, based on a survey distributed to haemophilia nurses across Europe [18, 19]. There are no similar studies within the United States HTC system.
Nurses comprise one of the largest components of HTC staffing, as evidenced by an inquiry into the Center for Disease Control (CDC) staff directory [20]. Multiple opportunities are available to receive specialised training in the management of bleeding disorders through programs such as the Partners Program™, Partners PRN™, and the Hemophilia of Georgia New Nurses Training Program [21]. However, there are very limited advanced training opportunities for APPs that support their specialised, advanced practice. Continuing education (CE) requirements vary from state to state, between professions (NPs vs. PAs) and between levels of professions (nurses vs. NPs) [22, 23].
While, in reality, APPs practice similarly on a day-today basis, their education (academic and clinical) and scope of practice is different [23]. Scope of practice varies from state to state. NPs are educated in the nursing and medical model, while PAs are educated solely in the medical model. Anecdotally, in HTCs, it is felt that APPs are trained by medical directors in a non-standardised fashion. Throughout this manuscript, PAs will be classified with NPs as APPs for ease of classification, with the above understanding noted. As APPs are filling the specialty physician void, there is recognition of a need to establish training programs (fellowships) to successfully acclimatise the APP to their new role [24, 25, 26, 27, 28]. Additionally, there are a number of new products being investigated and licensed which will refine the focus on personalised treatment. This will require even the most experienced haemophilia nurses to expand their knowledge base [29].
Aims
The primary aims of this study are to describe:
the demographics of all nurses within the HTC community
• the roles and responsibilities of APPs within the HTC community
the advanced training received to prepare these providers for their positions and support for development of an APP fellowship program
the barriers experienced by APPs to practicing in a subspecialty practice.
Methods
Study Design
The study is based on a one-time convenience online survey. A survey of this type had never been attempted in the US HTC nursing community; therefore, there was no opportunity to utilise a previous tool. The authors reviewed previous APRN benchmarking surveys from the American Association of Nurse Practitioners (AANP) and formulated a SurveyMonkey™ questionnaire based on these surveys, as well as the authors’ experiences/history and known issues within the community. The study was approved by the Munson Medical Center Institutional Review Board (IRB). Data was analysed using statistical tools through SurveyMonkey™ [30].
Recruitment Methods
Participants were HTC-employed registered nurses (RNs), APRNs and PAs identified through the NHF Nursing Work Group (NWG), CDC Bleeding Disorders Directory [20] and the mailing list for the Partners in Bleeding Disorders Education Program [21]. The eight ATHN regional coordinators were surveyed to verify that the list of nurses within their region was complete. A total of 438 potential participants were identified.
Survey
In March 2014, an introductory letter was emailed to participants alerting them to the forthcoming uncompensated survey. Six weekly reminders were emailed to those who did not complete their survey, with the option to opt out of further emails. No personal health information was collected.
Overall Results
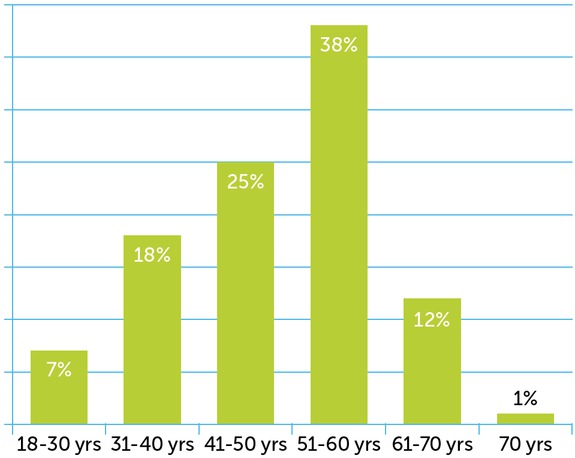
The survey was sent to 438 participants. The response rate was 42%, with a total of 186 respondents (%; n): RNs 71% (132), APRN-CNS 1% (2), APRN-NPs 26% (49), PAs 2% (3). The majority held a Bachelor’s Degree in Nursing (BSN) (42%; 78), followed by a Masters in Nursing (MSN) (34%; 63), Associates Degree in Nursing (ADN) (14%; 26), Diploma (9%; 16) and Doctorate (2%; 3). Of the 168 complete surveys, 38% (63) were in the 51-60 age group (see Table 1), 95% (159) female, 90% (151) white, 84% (141) working full-time, and 44% (74) held some type of national certification, most through the American Nurses Credentialing Center (ANCC). While 15% (26) of respondents did not have continuing education (CE) requirements within their state for licensure, 13% (21) had CE requirements for pain and 23% (38) had pharmacology CE requirements for continued state nursing licensure.
Table 1
Age distribution of all HTC respondents N=168
| 18-30 yrs | 7% |
|---|---|
| 31-40 yrs | 18% |
| 41-50 yrs | 25% |
| 51-60 yrs | 38% |
| 61-70 yrs | 12% |
| 70 yrs | 1% |
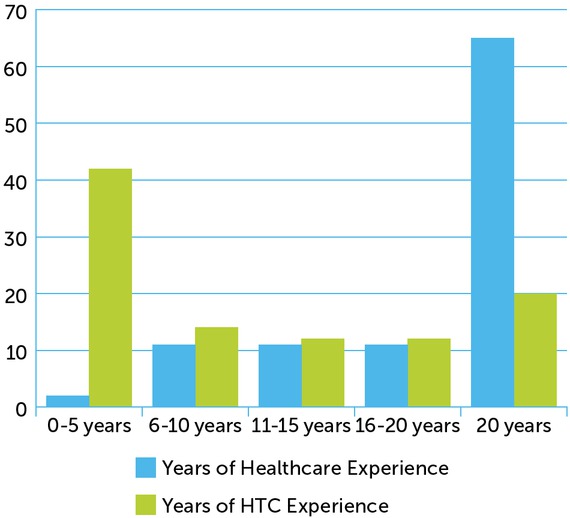
Although 65% (109) had more than 20 years of healthcare experience, 42% (70) had less than 5 years’ experience within the HTC system (Table 2). The distribution of respondents across all sizes of HTCs was fairly equal (>401 patients, 33% (56); 251-400 patients, 25% (43); 100-250 patients, 31% (52); <100 patients, 10% (17)), with the majority representing teaching institutions (74%; 24), treating the lifespan population (61%; 103), and both bleeding and thrombophilia disorders (73%; 122). The respondents’ HTCs funded the following positions: RN (65%; 110), data manager (57%; 96), research nurse (48%; 78) and NP (43%; 73). 56% (94) of respondents have no administrative duties in their job descriptions. The majority did not have protected time for any specific activities (62%; 104). Where there was protected time, this was specifically for education (31%; 52), administrative duties (16%; 27), research (15%; 25), advocacy (10%; 16) and publishing (3%; 5).
Table 2
Years of experience in healthcare compared to years of experience in HTCs
| YEARS OF HEALTHCARE EXPERIENCE | YEARS OF HTC EXPERIENCE | |
|---|---|---|
| 0-5 years | 2% | 42% |
| 6-10 years | 11% | 14% |
| 11-15 years | 11% | 12% |
| 16-20 years | 11% | 12% |
| 20 years | 65% | 20% |
| Total | 168 | 168 |
Despite the institutional restrictions experienced by 45% (76) of the respondents on the number or frequency of educational activities/development programs they could attend, a variety of training opportunities prepared respondents for their nursing HTC roles, including onsite preceptorship with an experienced HTC nurse (58%; 98), the Partners Program™ (55; 93), onsite preceptorship with a physician (40%; 67), the New Nurses Training Program in Atlanta, GA (32%; 54), online training through Partners PRN™ (20%; 34), industry-sponsored shadow program (7%; 11), and/or a mentor program (3%; 5). The top six ways HTC nurses become aware of important conferences to attend, working groups to participate in, or journals/articles to read were through their nursing colleagues (70%; 117), their regional coordinator (52%; 87), their physician colleagues (51%; 86), their regional colleagues (29%; 49), other staff members (29%; 48), and/or pharmaceutical representatives (28%; 47).
Respondents had minimal publishing experience, with 73% (123) never having published. Some published as the supporting author (24%; 40), first author (8%; 14) or sole author (2%; 4). Nearly half (44%; 75) have never presented at an educational meeting. Of those who have presented, 34% (57) presented at local meeting, 29% (49) presented at NHF and/or other professional meetings, 26% (44) presented at Chapter meetings and/or regional meetings, 21% (13) are on pharmaceutical speakers’ bureaus, 11% (19) presented on webinars, and 10% (17) presented internationally at the World Federation of Hemophilia (WFH) or International Society on Thrombosis and Haemostasis, Inc. (ISTH).
In the US, many HTCs receive revenue from the sale of factor concentrate to their patients through a pharmacy program. Only 13% (22) of respondents’ HTCs did not have a pharmacy program. In those HTCs with a pharmacy program, 47% (79) of respondents had no involvement. Of those who were involved, 15% (25) had input as to where revenues were utilised, 14% (24) had input on expenses of the program, and 20% (33) were responsible for growth of the program.
Respondents were asked about compensation and benefits based upon a full-time equivalent position. Most were in the $81-$90K income range 19% (32), followed by $61-70K and $71-80K 17% (28 each), $51-60K 13% (22), $91-100K 12% (20), $101-110K 10% (17), $121-130K 4% (7), <$50K and $111-120K 3% (5), >$141K 2% (3), $131-140K 1% (1).
When asked about benefits, 96% (162) received vacation, 86% (147) received health insurance, 76% (128) received retirement and travel to educational meetings/conferences, 66% (111) received CE reimbursement for professional development and conferences, 49% (83) received tuition reimbursement, 42% (71) received malpractice insurance coverage, 32% (53) received a pension, 24% (41) received reimbursement for their licensure/controlled drug substance certification (also known as Drug Enforcement Agency (DEA) certification), 20% (33) received reimbursement for professional association memberships, 11% (18) received bonus incentives, 7% (10) received on-call pay, and 4% (7) received reimbursement for moving expenses.
Advanced Practice Results
55 participants identified themselves as APRNs (nurse practitioners (NPs)/clinical nurse specialists (CNS)) or PAs. These providers were grouped together as APPs, but only 50 answered questions specific to their advanced practice, including whether they prescribed and what, whether they had a DEA license (72%; 36) and whether they maintained this in multiple states (12%; 6). Most APPs (58%; 29) were required by their states to have a collaborative agreement with a physician to prescribe medications, but 36% (18) practiced in states that allowed independent prescriptive authority.
Of the 50 prescribers, 94% (47) prescribed clotting factor, 76% (38) prescribed antithrombotic medications, 68% (34) prescribed Schedule III medications, 60% (30) prescribed Schedule II medications, and 58% (29) prescribed primary care non-scheduled medications, such as statins and hypertensive medications.
When asked to divide the percentage of their responsibilities as an APP, 50% of time was spent on direct patient care, followed by 17% telephone triage, 14% administrative, 8% research, 7% staff/provider education/precepting, 6% community events (camp/family meeting, etc.), 5% pharmacy program and 4% advocacy. APPs evaluate and manage patients independently, seeing them without a physician present and making treatment decisions, mostly for acute events (78%; 39) and follow-up visits (74%; 37). They also independently evaluate new patients (40%; 20) and inpatients (28%; 14). Only 14% (7) responded that they do not see/evaluate patients and make treatment decisions independently.
Answering calls from patients and families after hours is referred to as “taking call” or “being on-call”. Most APPs (74%; 37) responded that they do not take any call for their practice. Of those who do take call, 12% (6) take all call, 12% (6) take outpatient call only, and 2% (1) take inpatient only call. When taking call, 75% (9) are on-call less than 15 days per month, with 25% (3) on-call 16-30 days per month. Ten respondents reported receiving on-call pay as a benefit. Many APPs reported having additional responsibilities, including inpatient service (74%; 35) and performing procedures including, but not limited, to bone marrow aspirations (34%; 16). They are also called on to share their advanced level expertise by participating on advisory boards and committees, both within their institution (28%; 13) and outside their HTC (43%; 20).
Most APPs can bill insurance payers independently. In the US, a National Provider Identification (NPI) number is required to bill for services and to identify all providers [30]. APPs reported that they had provider numbers under their own names, including state and national insurance programs such as Medicaid (77%; 36) and Medicare (57%; 27). The majority billed under their own NPI (70%; 33). It was evenly divided as to whether metrics were used to measure productivity at their institution (40%; 19 each).
When asked about monetary compensation at the time of accepting their position as an APP, 38% (18) of NPs received additional compensation for previous experience as a RN, while 26% (12) only received compensation for previous experience as an NP and 38% (18) did not receive any additional compensation for previous experience of any kind. Those with a doctorate did not receive additional compensation for their higher degree. Sign-on bonuses were rare (6%; 3).
Discussion
Demographics and Roles of RNs/APRNs/PAs Within the HTC Community
Multidisciplinary team (MDT) care, as provided in the HTC model, is a team-based systems approach to providing healthcare delivery, through communicated care, coordinated information sharing, and cooperative partnerships of various healthcare professionals, patients and their families. With the establishment of the HTC network in the 1970s, the MDT model was adopted with demonstrated overall improvements for patients with haemophilia [4]. The US Institute of Medicine (IOM) has stated that the concept of team-based care is “the provision of health services to individuals, families, and/or their communities by at least two health providers who work collaboratively, to the extent preferred by each patient. The purpose of Team Based Care is to provide coordinated, high quality, and patient-centred care” [7]. While nursing practice is at the foundation of the HTC MDT and exemplifies the essential characteristics of communicated, coordinated and cooperative care that is required in a team-based healthcare approach, there has not been a detailed description of the demographics or roles of nurses in the US HTC setting.
This survey revealed an aging nursing population, with over 50% of the respondents over the age of 50, experienced in healthcare but newer to the field of bleeding disorders. They were also highly educated, with the majority holding at least a baccalaureate degree and almost half with national board certification. Involvement in advisory boards and committees reflects the clinical expertise of the group. The practice patterns of the nurses were not surveyed in depth. The practice patterns of the APPs who responded to this survey consisted of mostly clinical roles at teaching institutions specialising in both bleeding and clotting disorders, with various roles within an HTC described as direct patient care, educator, research coordinator, program coordinator, administrator and manager. Both roles (nurse and APP) are necessary for the future of comprehensive care in the HTC setting, with distinctly different responsibilities.
Salaries and compensation varied based on education level, years of experience and institutional benefit packages. There was little relationship between years at the HTC and salary. Those with less than five years’ experience were found in all salary ranges, as were those with more than 20 years’ experience at the HTC. Compensation increased in line with educational level, with 63% of master’s prepared nurses and 100% of doctoral prepared nurses receiving more than US$100,000 per year, 67% of bachelor’s prepared nurses receiving between US$61-90,000 per year, and 65% of associate prepared nurses receiving less than US$70,000 per year.
Advanced Training Received to Prepare APPs for their Positions
Knowledge and information is acquired though continued education, on-the-job learning, and mentorship of experienced practitioners. State licensure requires continuing education, with a growing focus in pharmacology and pain management, demonstrating the need for standardised programs. This survey revealed that the specialised education of HTC nurses is an uncoordinated mix of on-site institution-specific training/mentorship by a physician/nurse, and through one particular curriculum-based program, the Medical and Scientific Advisory Council (MASAC)-endorsed Partners in Bleeding Disorders Education™, in addition to other symposia [21]. The Partners program objectives are “to describe the pathophysiology of haemophilia, its underlying genetics, basic treatments, and possible complications” [32].
Sources of information for training come from nursing colleagues, regional coordinators and HTC physicians. The educational preparation and training of the APP was focused more on the medical model and generally delivered by the on-site physician, with no standardised curriculum. APPs reported minimal involvement in a mentoring program.
Support for Advanced Practice Nursing
In the IOM’s 2010 landmark publication, The Future of Nursing, significant recommendations were outlined that propelled the profession of nursing, and the advanced practice role specifically, to the forefront in shaping the delivery of healthcare in the United States [7]. Historically, nurses have been the frontline for patient contact, and in the HTC model are at its core. The IOM document recognises and supports and recognises the need for the unique skills presented by the profession to advance the responsibilities and roles of the nurse. Four key messages were identified:
Barriers to nursing practice need to be removed to enable nurses to practice to the fullest extent of education
Improved seamless educational systems are needed to allow for higher levels of nursing education
Full partnership between nurses and physicians should be allowed
Data collection and information infrastructure must be improved to create effective workforce planning and policy making.
This survey demonstrates the active utilisation of APPs in the comprehensive care model of the HTC. The specific APP role was reported to include direct patient care, phone triage, research and administrative responsibilities. Under the Title 21 US Code Controlled Substance Act, any person in the US who dispenses a controlled substance must register with the government and receive a Controlled Drug Substance (CDS) number and Drug Enforcement Agency (DEA) number [33]. Most APPs reported having a CDS number and state licensure from the DEA in at least one state, with either independent prescriptive authority or delegated authority through a collaborative agreement with a physician. Medications commonly prescribed included clotting factor concentrates, antithrombotic medications and Schedule II-V medications, reflecting the needs of the populations served. Most APPs report the availability of a physician on site, but some report autonomous practice [12]. The majority report independent patient management of acute events and follow-up visits, and to a lesser extent, new patient and inpatient visits. Over 70% of APPs bill independently. Only half stated that their productivity is measured by billable encounters.
One role of the APP is research, which is critical in furthering evidence-based nursing practice [26]. Over half of respondents report having no protected time to conduct or participate in nursing research. Those with protected time are involved in research and publishing, ranging from sole authorship to supporting authors and involvement in peer review journals. A focus on evidence-based research will be critical as nurses and APPs within the HTC community improve patient care and outcomes.
Limitations
This was an anonymous convenience study which provided a snapshot of the HTC nursing landscape at a point in time. As healthcare rapidly evolves, roles and responsibilities evolve quickly, as does the need to monitor and identify trends and barriers. The survey did not define role responsibilities for the US HTC nurse. Future surveys will define and delineate that role more precisely.
Conclusion
The subspecialty of bleeding disorders nursing requires specialised knowledge, skill and independent decision-making. In our survey, over a third of the nurses will reach retirement age in the next 10-15 years, thus increasing the urgency of efforts to create a standardised approach toward education, with the goal of supporting recruitment and retention.
One challenge to education standardisation is that, unlike other subspecialty nursing areas, there is not an independent nursing society guiding the curriculum. Without this, progress toward standardisation of education is slow and sometimes disjointed. Over half of the nurses surveyed did not report restriction on educational or developmental programs as a barrier, indicating that participation in additional educational initiatives would be supported.
A barrier is the small number of HTC nurses compared to other subspecialties, such as diabetes or oncology. The Hemostasis Nursing board certification, which became available in December 2015, is a step towards the standardisation of competencies. The curriculum developed by the EAHAD Nurses’ Committee would also be an excellent resource for the US nurses to use as a template [19]. Further development of an APP fellowship program would standardise the care and treatment of those with bleeding and clotting disorders across the United States. This fellowship should be developed by experienced APPs currently practicing in the field, and include a didactic portion to include differential diagnosis, diagnostic testing and tools, assessment, treatment options, evaluation, research opportunities and patient outcome studies. Advocacy within the community is also important, including advocacy for the consumer, the community and for nursing. Mentorship with other more experienced APRNs would be advantageous, as would regular webinar-based case studies to review current trends in care.
There is high demand for sub-specialised care for the bleeding disorders community. To continue providing the high level of care required by this population, further standardised education will be required for the APP. This survey is a call to action to begin standardised education programs for the advanced practice role.