Nurses play a pivotal role in providing comprehensive care to people with haemophilia and related disorders and coordinating care with other members of the multidisciplinary team, both within hospitals, the community and the patient’s own homes.
Clinical nurse specialists in haemophilia and related disorders are advanced practitioners with extensive clinical knowledge and expertise in this specialist field. Nurses use their clinical, communication and interpersonal skills to identify the needs of people with haemophilia and related disorders and to provide care that recognises social, cultural and spiritual differences throughout a person’s life.
Advanced nursing roles within haemophilia in the UK include advanced nurse practitioners; a role recognized by attaining a masters level in advancing nursing practice at accredited universities, clinical nurse specialists and consultant nurses. Clinical nurse specialists are recognized as having five principal functions that encompass clinical practice, advocacy, advice, education and research [1,2]. The key components of the haemophilia nurse consultant role are expert practice, leadership and consultancy, education and training and research and evaluation. To fulfill these roles nurses must be confident and competent.
Competency is the combination of attributes, knowledge and skills that underpin professional practice [3].
Development of competencies should help individuals to continually improve their performance and to work more effectively [4]. A ‘competency framework’ is a structure that sets out and defines each individual competency (such as problem-solving or people management) thought to be central to effective performance and therefore required of individuals and nursing teams.
Competency-based approaches have been widely advocated both to ensure fitness for practice [5,6] and to promote professional and personal development among specialist nurses in the United Kingdom (UK)[8]. As a key part of Agenda for Change – a UK National Health Service (NHS) initiative introduced in 2004, including annual appraisal and personal development plans, linked to pay – the NHS developed a Knowledge and Skills Framework (KSF) under which all nursing staff should:
have clear and consistent development objectives
be helped to develop in such a way that they can apply the knowledge and skills appropriate to their level of responsibility
be helped to identify and develop knowledge and skills that will support their career progression.
In order to help nurses fulfill their role, in 2002 members of the United Kingdom’s Haemophilia Nurses’ Association (HNA) devised a paper-based, hand-held core competency framework that defined differing levels of haemophilia nursing intervention in key aspects of care. This could be used for individual haemophilia nurses to inform personal development plans as well as teams of nurses in haemophilia centres to develop strategic visions for future service provision. This was subsequently revised and expanded into an electronic tool, stored on a secure website (www.haemnet.com) supported by the HNA. This paper describes the process by which the framework was developed and summarises the core attributes expected of this group of highly specialized nurses.
Analysis
Under the auspices of the HNA, a working party of experienced nurses (MB, DE, KK, NM) was convened, which reflected the plurality of experience, specialism, age focus and geographical location of haemophilia nurses in the UK. The group sought to:
Identify an agreed theoretical premise of competency
Describe different aspects of haemophilia nurse intervention
Map differing levels of expertise within these aspects using descriptors drawn from nursing theory.
Benner introduced the concept that nurses develop skills and understanding of patient care over time through a sound educational base as well as experience [8]. The HNA focus group assessed clinical nursing practice using a variation of this system based on five practice domains:
Knowledge
Action
Problem solving /management decision making
Interpersonal communication
Self-management/reflection
These were measured against four levels of practice and academic indicators derived from Benner [8]:
Novice/advanced beginner (Level 1 certificate)
Competent (Level 2 diploma)
Proficient (Level 3 degree)
Expert/specialist nurse (Masters Level and beyond)
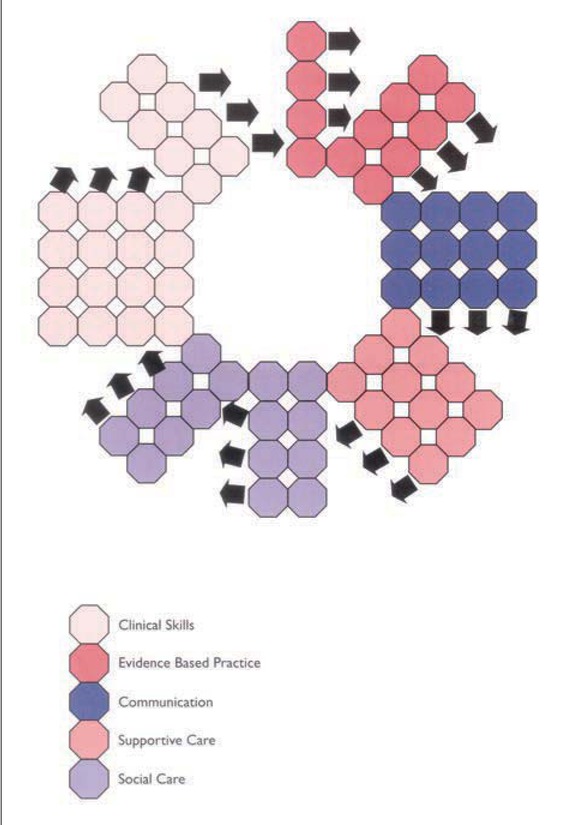
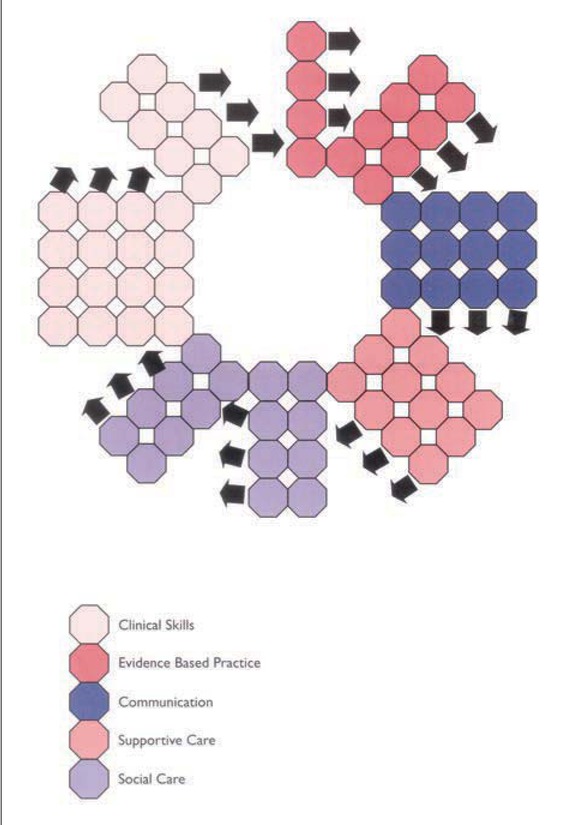
The working party considered key events along a lifelong patient pathway and grouped these into aspects of practice. These areas were then collated into five core frames of practice (clinical skills, evidence-based practice, communication, supportive care, and social care). Each of these frames was to be considered by individual nurses in terms of their achieved levels of practice. Mapping these descriptors onto an assessment grid (known as a Stepford Spiral, Figure 1) provides individual nurses with a visual representation of their achieved competency as well as their required areas of development.
Figure 1
The framework was designed to be used for:
Self-appraisal, to identify learning needs.
Within the personal review process to help staff development.
Strategically, to identify team skills mix.
For quality assurance and audit purposes (locally or nationally) to define a requisite nursing profile for different types of haemophilia centre (haemophilia centre vs comprehensive care centre etc).
In 2009 the framework was revised to reflect the growing role of haemophilia clinical nurse specialists and consultant nurses [9]. The new competency framework includes additional knowledge domains in six ‘satellite competencies’: children and young people, inhibitor management/care, clinical care, leadership skills, genetic knowledge and skills, and women’s issues.
Results and discussion
The HNA competency framework currently consists of five core domains (communication, research, education, support and treatment; Table 1) and an additional six “satellite” domains (women, children, leadership, inhibitors, genetics and physiotherapy; Table 2). Each level of the framework cites key references and links to the Department of Health Knowledge Skills Framework.
Table 1
The core competency domains
|
Level 1 |
Level 2 |
Level 3 |
Level 4 |
|
COMMUNICATION
|
|
Haemophilia MDT |
Demonstrates understanding of the role of team members and communicates appropriately. Is able to observe and report accurately |
Presents cases and raises issues within the team |
Initiates and leads team discussions |
|
|
Liaison and referral |
Liaises with referral agencies under supervision. Demonstrates a working knowledge of the range of specialist services available |
Makes referral within the HMDT. Supervises care provision and requirements of individuals needing multi-agency services |
Represents the HMDT in multiagency settings |
Makes referral to services outside the HMDT. Negotiates improved service provision and resource allocation for people with bleeding disorders |
|
Interpersonal communication |
Communicates effectively within familiar situations |
Communicates effectively in a variety of ways and situations |
Can mediate and manage conflict |
Facilitates the development of others appropriate to needs of patients and their families |
|
RESEARCH
|
|
Audit and resource skills |
Avoids wasteful use of resources. Recognises need for data collection in haemophilia management |
Audits procedures, policies and protocols |
Understands the implication of audit data and uses this to effectively manage resources |
Develops audit procedures and uses audit data to improve service delivery |
|
EDUCATION
|
|
Education |
Can explain basic haemophilia care and management in a one-to-one setting |
Can teach and assess in clinical situations and supports other agencies |
Plans and delivers teaching interventions |
Strategically evaluates education needs and develops responsive programmes |
|
Training for home therapy |
Participates, under supervision, with teaching and training |
Implements individual home treatment training |
Manages and evaluates training programmes |
Develops training programmes and facilitates best practice |
|
SUPPORT
|
|
Advocacy |
Recognises the impact that legal and ethical concerns have on the practice of nursing e.g. reproductive choices. Supports the patient and family in the decision making process |
Enables patients and their family to make informed health care decisions |
Takes leadership role in patient advocacy |
Recognises emerging ethical and legal issues and initiates discussion at a professional level |
|
Cultural and spiritual |
Aware of the issues that underpin individual spiritual views |
Can assess the potential impact of illness on patient’s lifestyle, cultural beliefs and support systems |
Facilitates discussion in relation to spiritual and cultural issues |
Organises appropriate support mechanisms for those involved in spiritual/cultural care |
|
Clinical supervision |
Uses clinical supervision to critically reflect upon their developing clinical expertise |
Uses clinical supervision skills in the development of others |
|
|
|
Counselling skills |
Has effective listening skills, and develops therapeutic relationships |
Manages emotionally taxing situations |
Is responsive to patients coping’ mechanisms |
Is confident to challenge dysfunctional behaviour |
|
TREATMENT
|
|
Diagnostic skills |
Recognises signs and symptoms of bleeding at common sites |
Has a detailed knowledge of pathophysiology to explain presenting symptoms |
Assesses physiological functioning and develops intervention plan |
Determines differential diagnoses, using examination and investigations |
|
Factor replacement skills |
Performs venepuncture in non-problematic situations |
Performs venepuncture in more problematic situations. Administers coagulation factors |
Formulates a care plan in liaison with other members of the HMDT. Co-ordinates more complex clinical interventions |
Prescribes replacement therapy |
|
Clinical decision making |
Participates, under supervision, in decision-making |
Makes decisions in predictable situations |
Facilitates decision-making within the HMDT |
Initiates innovative practice |
Table 2
The five satellite competency domains
|
Level 1 |
Level 2 |
Level 3 |
Level 4 |
|
CHILDREN AND YOUNG PEOPLE
|
|
Monitoring health |
Communicates with children and young people in an age/developmentally appropriate manner |
Observes the behaviour of children and young people and records unexpected changes and concerns |
Demonstrates listening and responds appropriately to issues raised by children and young people |
Recognises child assent/consent process and acts as children and young people advocate |
|
Enabling children and young people to understand health care needs |
Discusses children and young people’s views on health and well-being |
Provides evidence-based care and information to children and young people and their families |
Supports children and young people and their families in a partnership based model of care |
Enables children and young people to communicate issues of health, treatment and care |
|
Supporting children and young people in medicine/treatment management |
Advises children and young people and their families about managing coagulation factors |
nables children and young people and families to monitor treatment planning and response |
Advises children and young people and their families about factor storage, use, transportation and disposal |
|
|
Supporting adolescent transition |
Provides suitable information about transition from paediatric to adult care |
Provides suitable information about transition from paediatric to adult care |
Reviews self-management skills of young people to support adult care after transition |
Ensures smooth transition from paediatric care/hospital to adult care/hospital |
|
INHIBITORS
|
|
Recognises risk factors for inhibitor development |
Describes screening/detection protocols |
Demonstrates detailed knowledge of presenting symptoms and laboratory results |
Assesses treatment response and develops treatment plans for bleed management |
|
Works as part of a team promoting equity in the decision-making process. Supports and motivates other team members |
Empowers, motivates and supports others to develop their clinical skills. Takes responsibility for the actions of junior staff |
Develops a culture of continuing development and improvement of clinical skills. Promotes autonomy while ensuring the quality and safety of patient care. Takes responsibility for the service-wide quality of care |
|
|
CLINICAL LEADERSHIP
|
|
History taking |
Take a simple family history of common bleeding disorders and draw a family tree |
Take complex history of common bleeding disorders and draw a family tree |
Take history of complex bleeding disorders and draw a family tree |
|
|
Identifying those at risk |
Identify patterns of inheritance in common bleeding disorders |
Identify patterns of inheritance in complex bleeding disorders |
Use family history to identify patients with or at risk of a bleeding disorder and refer as appropriate |
|
|
Intervention |
Recognise the impact that genetic information may have on individuals and families |
Explain basic modes of inheritance to patients and families |
Apply detailed genetic knowledge to inform treatment in complex situations |
Order genetic tests and communicate results to patients and families |
|
WOMEN WITH BLEEDING DISORDERS AND MENNORHAGIA
|
|
Monitoring health |
Identifies the risk factors to health for women with bleeding disorders |
Describes the screening tools available to assess women presenting with menorrhagia |
Demonstrates detailed knowledge of presenting symptoms of menorrhagia in women with bleeding disorders |
Independently assesses women with bleeding disorders, initiating appropriate screening tests and making further referrals |
|
Education and management needs |
Discusses individual’s views and knowledge of their condition |
Provides evidence-based care and information to women |
Supports women to make informed choices regarding treatment and management |
Enables women to independently manage bleeding symptoms where appropriate and provides a pathway for when further health care is required |
|
Perinatal care and management |
Recognizes the risk factors for women with bleeding disorders through the peri-natal period and understands which situations require urgent referral |
Describes the ante-natal care pathways for carriers of haemophilia and women with bleeding disorders |
Demonstrates detailed knowledge of the physical, psychological and emotional needs of carriers of haemophilia and women with bleeding disorders |
Enables women to make informed choices about peri-natal care and to communicate their needs to other healthcare professionals |
An online version of the framework is now available on Haemnet (www.haemnet.com) This allows nurses, over a period of time, to:
Launched in 2010, over 200 nurses have registered on Haemnet and many UK-based nurses have used the online framework.
The competency framework establishes a baseline educational and practical skills forum for nurses new to haemophilia, which allows progression through personalized development and assessment, to competence at all levels of haemophilia nursing. Many aspects of the framework include transferrable skills such as communication skills, so even ‘novice’ haemophilia nurses are part way along the road to haemophilia competence.
This tool can be used as part of both formal (manager appraisal, objective setting etc) and informal (own assessment) development identifying areas for further education and learning. Although the UK HNA developed this tool, based on UK nurse training/education models there is no reason why it cannot be applied, perhaps in adapted forms, globally. In this journal, Schrjivers et al suggest that European haemophilia nursing curricula and European principles for haemophilia nursing care should be developed [10]. Modification of the competency framework, in line with local/national nurse education/legal programmes would go along way towards this. As well as continuing to develop shared practice across the EU.
Conclusion
Haemophilia nursing is a complex art; weaving knowledge and skills with scientific doctrine to promote evidence based care, advocacy and self-management skills for people with bleeding disorders. Whilst many legal standards impact upon the role of the nurse across countries, we share more than we realize. The principles of nursing care for patients with bleeding disorders are the same regardless of your language; we care, support, listen, educate, advocate, research and publish. Sharing best practice with fellow nurses impacts beyond the borders of our own hospitals/treatment centres and countries leading to empowered nursing communities globally – come on join in!
Acknowledgement
The authors wish to thank all of the clinical nurse specialists who helped in the development of the HNA framework. The original work to develop the paper-based framework was sponsored by Wyeth UK, and development of the updated electronic framework was supported by Pfizer UK
References
Manley K. A conceptual framework for advanced practice: an action research project operationalizing an advanced practitioner/ consultant nurse role. J Clin Nurs 1997; 6: 179–90.
K ManleyA conceptual framework for advanced practice: an action research project operationalizing an advanced practitioner/ consultant nurse roleJ Clin Nurs1997617990
Macdonald JA, Herbert R, Thibeault C. Advanced practice nursing: unification through a common identity. J Prof Nurs 2006; 22: 172–9.
JA MacdonaldR HerbertC ThibeaultAdvanced practice nursing: unification through a common identityJ Prof Nurs2006221729
Fish D, Purr B. An Evaluation of Practice-Based Learning in Continuing Professional Education in Nursing , Midwifery and Health Visiting London: ENB, 1991.
D FishB PurrAn Evaluation of Practice-Based Learning in Continuing Professional Education in Nursing , Midwifery and Health VisitingLondonENB1991
Whiddett S, Hollyforde, S. The Competencies Handbook Institute of Personnel and Development, 1999.
S WhiddettS HollyfordeThe Competencies HandbookInstitute of Personnel and Development1999
United Kingdom Central Council for Nursing, Midwifery and Health Visiting. Fitness for Practice: The UKCC Commission for Nursing and Midwifery Education UKCC, 1999.
United Kingdom Central Council for Nursing, Midwifery and Health VisitingFitness for Practice: The UKCC Commission for Nursing and Midwifery EducationUKCC1999
Burke S, Barker C, Marshall D. Developing education tailored to clinical roles: genetics education for haemophilia nurses Nurse Educ Today 2012; 32(1): 52-6.
S BurkeC BarkerD MarshallDeveloping education tailored to clinical roles: genetics education for haemophilia nurses Nurse Educ Today2012321526
Department of Health. The NHS Knowledge and Skills Framework (NHS KSF) and the Development Review Process London, DoH, October 2004.
Department of HealthThe NHS Knowledge and Skills Framework (NHS KSF) and the Development Review ProcessLondonDoH2004
Benner P. From Novice to Expert: Excellence and Power in Clinical Nursing Practice Menlo Park, CA: Addison-Wesley, 1984.
P BennerFrom Novice to Expert: Excellence and Power in Clinical Nursing PracticeMenlo Park, CAAddison-Wesley1984
Gregorowski A, Brennan E, Chapman S, Gibson F, Khair K, May L, Lindsay-Waters A. An action research study to explore the nature of the nurse consultant role in the care of children and young people. J Clin Nurs 2013; 22(1-2): 201-10.
A GregorowskiE BrennanS ChapmanF GibsonK KhairL MayA Lindsay-WatersAn action research study to explore the nature of the nurse consultant role in the care of children and young peopleJ Clin Nurs2013221-220110
Schrijvers LH, Bedford M, Elfvinge P, et al. On behalf of the EAHAD nurses committee. The role of the European haemophilia nurse. J Haem Pract 2014; 1(1): 24-27.
LH SchrijversM BedfordP Elfvingeet alOn behalf of the EAHAD nurses committee. The role of the European haemophilia nurseJ Haem Pract2014112427